Article • Focus on quality control
Improving radiology department efficiency for hospital inpatients
Because radiology exams are an integral part of the treatment process for many hospital inpatients, any improvements in efficiency can have a positive ripple effect on routine hospital operations and functionality. Two quality control presentations at the 2023 RSNA Annual Meeting shared the theme of creating representational staff teams to identify bottlenecks involving radiology report turnaround times. Using structured quality improvement methodologies, they developed and tested practical potential solutions, and recorded the results. Their changes, resulting in positive improvements, merit evaluation and testing in hospitals with similar issues.
Report: Cynthia E. Keen

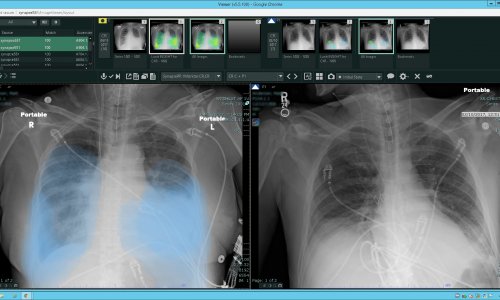
Should all portable exams ordered for paediatric cardiac intensive care unit (CICU) patients be designated as STAT? At Children’s Hospital of Philadelphia, most ICU portable exams were being requested as high priority STAT exams without considering the urgency of their need. This resulted in inefficiencies in processing the radiology findings of highest priority patents to their ordering physicians.
‘If everything is STAT, nothing is STAT, because the radiographer team for portable X-ray exams is unable to respond to simultaneous requests,’ explained radiology quality assurance technologist Eatrice Y. Hinton, AS RT R. ‘Radiographers had to make decisions without clinical input on whom to image first, and this was causing us stress.’
A multidisciplinary team of clinicians and staff members from the radiology department and the CICU was assembled with the goal of reducing the time to take portable exams of high priority patients. The team included physicians, technologists, nurses, a human factors engineer, and a safety and quality specialist, who collectively observed and recorded every step of the process in detail. They identified three major factors. The radiographers were consistently busy. Priorities were being communicated by telephone and did not always happen or required multiple calls for clarification. Radiographers also did not have access to the patient’s electronic medical record (EMR) at the hospital.
Interventions included creating a well-defined clinical criteria list for prioritizing STAT orders and to prevent inappropriate labelling of non-STAT cases. The hospital implemented a new secure chat text messaging system between ordering physicians and CICU radiographers for direct communication. Six months after implementation, turnaround time between order and exam completion was reduced from a median of 24 minutes to 15 minutes.
‘The relationship and communications between the CICU teams and radiology teams have improved,’ Hinton tells Healthcare in Europe. ‘Our new process has been implemented in the CICU step-down unit and in the Neonatal Intensive Care Unit. We are currently investigating the clinical criteria needed for implementation in the paediatric ICU and customising it for that portable radiology team’s specific clinical needs.’

© alexlmx – stock.adobe.com
Reducing turnaround time for routine inpatient neurology MRI reports
The Main Line Health System, serving portions of Philadelphia, Pennsylvania, and its western suburbs, is focused on reducing the length of stay (LOS) of its inpatients to reduce healthcare costs, and has been using its EMR to improve systemwide processes to do so.

‘We believe that the Radiology Department has an important role to play in influencing the length of stay,’ said radiologist Ashima Lall, MD. ‘We had anecdotal evidence that inpatients with neurological diagnosis might have higher length of stay because they were waiting for final imaging results after routine MRI studies.’
So the hospital system created an interdisciplinary professional team to analyze data, troubleshoot, identify barriers, and design a pilot program to resolve them. During its investigation, the team had discovered that the EMR did not alert the radiology department of routine inpatient studies on patients awaiting MRI results to be discharged.
To overcome this, the team developed a “demand signal” in the EMR to identify patients who could be discharged within 24 hours following receipt of MRI imaging results. They expected that this additional EMR functionality would help radiographers and radiologists prioritize routine orders of these inpatients ahead of other routine inpatient studies.
Proper selection of imaging studies for demand signal use by an interprofessional team is important and should be data-driven. It may vary at other institutions
Ashima Lall
A six-month long pilot study of neurology patients using the demand signal across all four hospitals was launched in March 2022. Discharge results were compared with baseline metrics from May 2020 through May 2021. With the change, the average time reduction between the order for the MRI and the time it was performed was 9 minutes compared to 17 minutes, and the average time from the MRI to report dictation was 3.1 minutes compared to 4.55 minutes. Impressively, the average time to discharge for this patient group was halved. This initial pilot data showed that 51% of these demand signal patients were discharged in less than 24 hours and 70% within 48 hours. They were associated with 300 fewer inpatient days and 34.5 observation days compared to the controls.
The team calculated that the cost savings during the pilot study was US $42,649, and US $170,595 if projected to a year. Another benefit is that inpatient beds are becoming available more rapidly for admitted emergency patients. Data is reviewed monthly to ensure that there is no deviation from the process or significant variation from expected projections. ‘We continue to use the demand signal in all four hospitals’, Lall advises. ’In 2023, the Main Line Health System scaled this approach to other imaging modalities like CT and ultrasound.’
She tells Healthcare in Europe that after analyzing six months of the data, the demand signal was expanded to CT and ultrasound procedures that were associated with the largest numbers of patients discharged within 48 hours after receiving imaging results back. These selected procedures included imaging studies in both Neuro and Body Imaging.
‘Proper selection of imaging studies for demand signal use by an interprofessional team is important and should be data-driven. It may vary at other institutions. This should be emphasized for optimal resource use as it is one of the important drivers influencing the outcome,’ cautions Lall.
03.10.2024