Predictive analysis
USA healthcare recognises electronic benefits for patient care – and lower costs
The USA’s healthcare system has awakened to the fact that electronically stored health patient data can save billions of dollars. Predictive analysis of ‘Big Data’ is a hot topic.The USA’s healthcare system has awakened to the fact that electronically stored health patient data can save billions of dollars. Predictive analysis of ‘Big Data’ is a hot topic.

Although in its infancy in terms of healthcare application, an impressive amount of governmental, organisational, corporate and venture funds are being invested in this technology.
Predictive analytics is a statistical technique that uses data mining and modelling to identify trends and predict outcomes. Predictive models are used to analyse historical and current data to identify detailed trends, risks, probability levels, and opportunities for hospitals to improve their services and patient outcomes.
In July 2013, the USA’s National Institutes of Health (NIH) committed $96 million ($24 million annually) to establish six to eight Big Data Knowledge Centres of Excellence. These have a mandate to develop and distribute innovative approaches, methods, software and tools for data sharing, integration, analysis and management. The resulting innovations are intended to make it easier for healthcare providers to manage big data, a problem that NIH believes is due to a lack of tools.
Big business agrees. Just one example of funds being invested in companies developing predictive analytics software for healthcare applications: recently Predixion Software of San Juan Capistrano, California raised $20 million. The primary investors were Accenture, EMC, and GE Ventures. T
The Advisory Board Company, an international consultancy, purchased Silicon Valley clinical analytics company 360Fresh to augment its Crimson software. Crimson’s software tools allow hospitals to track complications, readmissions, and cost measures for each physician, as well as do peer review analysis. The Advisory Board Company’s acquisition integrated software capable of extracting information from existing systems such as electronic medical records. Its data mining functions and analytics functions use text analytics and neuro-linguistic programming (NLP) processing to analyse both structured and unstructured data. This can include progress notes, admissions records, treatment regimes, and outcomes. This data can be used to create a comprehensive view of potential risk factors for individual patients.
The motto of Predixion Software is ‘You cannot prevent what you cannot predict’. Hospitals in the United Kingdom and United States are fined if patients’ readmission levels exceed a defined threshold. Using data of comparable patients, a predictive model can identify at-risk patients admitted to hospital for the first time. Risks of individual patients can be stratified daily, and treatment interventions can be implemented promptly. Analytic tools are also particularly useful in hospital efforts to reduce sepsis, decubitus ulcers, and in-patient mortality.
Hospital enterprises like NorthShore University Health System and Rush University Medical Centre, in metropolitan Chicago, use models to assign risk levels of patients who have had, or are at risk of having, a stroke or cardiac arrest. When patients are admitted to Rush’s emergency department with these symptoms who fit a high-risk profile, emergency physicians immediately notify cardiologists. Since time to treatment vitally affects outcomes of heart attack and stroke victims, use of the model eliminates delays waiting for treatment in the emergency department for patients assigned to a highest risk quartile.
Predictive analytics goes beyond analysis of just clinical information. It also factors in the age of the patient, availability of personal caregivers, transportation access, financial wherewithal to purchase prescription drugs, and available community resources that may greatly differ in urban and rural areas. These out-patient variables tend to be far more heterogeneous than in-patient variables. Medical providers can then customise a programme of care for the patient, so that re-admissions can be avoided or significantly reduced.
Predictive analysis is also starting to be used to supplement clinical trials intending to determine how a prescription medication or clinical treatment will work. This is being used to support the development and use of evidence-based medicine. It also can analyse a patient population based on multiple co-morbidities.
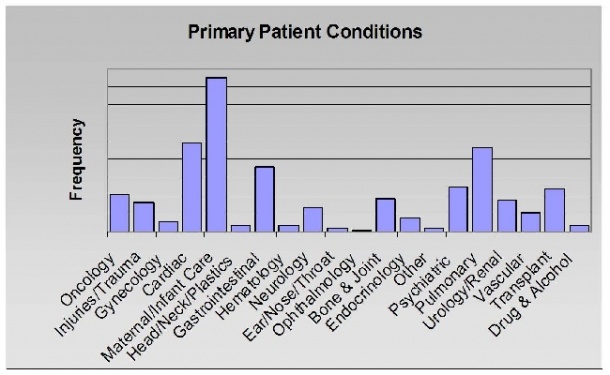
‘Current economic reimbursement models for USA hospitals only consider clinical intervention assuming a simple view of service volumes (see Figure 1). However, a percentage of patients have co-morbidities,’ explained Paul Savage, president of Healthcare Intelligence, a predictive analytics consultancy in Old Greenwich, Connecticut. ‘It’s important to understand the entire scope of what clinicians are treating and the underlying prevalence of chronic diseases, such as diabetes, even if these are not the immediate cause of an episode of treatment. With this understanding, the epidemiology of population health can be modelled recognising the trends and seasonality of patient needs and resource consumption.’ [Figure 2 shows the realistic patient mix.]
Predictive analytics models can be honed to population demographics, geographic region, and even time of year. Their predictive accuracy can be checked against subsequent historic data. In a 2012 interview with healthcare IT blogger HIStalk (ww.histalk2.com) a Mr Arkell observed that ‘being able to assign a risk profile to specific patients when they admit the first time is something that’s a game-changing solution’. Healthcare providers who begin to use the technology tend to agree. Expect the use of predictive analytics to proliferate.
18.11.2013






