Patient data transfer and healthcare policy-making
Now central to most medical and policy-making discussions, cross-border healthcare, telemedicine and e-health are a top priority on the EU’s healthcare agenda, and most Member States are working to develop viable systems in this field

During a recent presentation at the EMMIT conference in Malta, Dr Mario Ciampi, researcher into software architecture for e-health at the Istituto di Calcolo e Reti ad Alte Prestazioni (ICAR) in Naples, gave an account of Italian efforts to introduce e-health on a national level. This member state is working on three main e-Health initiatives: e-prescription, online sick notes and medical reports, aiming to collect and store relevant data in repositories and harmonise communication between the parties involved. In fact, most of the regional administrations have started a series of initiatives to set up Electronic Health Record (EHR) systems. However, unfortunately each region is setting up its own system, adopting heterogeneous architectural and technological set-ups and thus not only is progress uneven overall but interoperability is also hindered.
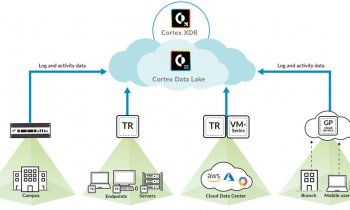
In his capacity as a researcher summed up: ‘Compared to the general domain text, information extraction from unstructured clinical data has been lagging behind, at the National Research Council of Italy (CNR), of which his institute is part, Dr Ciampi also talked about projects, coordinated by Dr Giuseppe De Pietro, which were launched in an attempt to set up a functional e-health system at a national level. The first, InFSE, a joint project between the Research Centre and the Presidency of the Council of Ministers of Italy, ran from May 2009 to October 2010 and aimed at setting up the technological infrastructure of EHRs. This infrastructure includes an Access Interface, found both at local and regional nodes. This allows interactions between the local domain and the infrastructure and provides all necessary functions to search for, obtain or publish a health document. It also includes a Federated Index Registry, made up of the regional registries, a Document Manager that allows storage and retrieval of documents by an authorised user, a Hierarchical Event Manager, able to notify clinical events, and an Access Policy Manager, which deals with authentication, identification and authorisation mechanisms. This InFSE architectural model has also been outlined in detail in guidelines that have been incorporated in the ‘Guidelines on Electronic Health Record, produced by the Italian Health Ministry.
OpenInFSE success
The OpenInFSE project followed suite, aimed at the setting up of an operational infrastructure to support the interoperability of EHR in the context of the Public System Connectivity. Three regions, namely Piedmont, Campania and Calabria, were involved in this project, which not only worked at implementing and sharing InFSE components with Web Services Technology but also at integrating these components with regional EHR systems and it experimented with the interchange of healthcare documents between the three regions involved.
The setup of the OpenInFSE project laid the groundwork for the IPSE project, which involved a greater number of regions and provinces in the Italian peninsula and experimented with the exchange of patient summaries by interoperability of regional EHR systems. Connected to the epSOS project (European Patient - Smart Open Services) this project allowed for both direct (region known) and federated (region unknown) search of patient records and for document retrieval.
The Italian e-health pipeline is still buzzing with activity with ongoing and prospective projects cofinanced by the Presidency and the National Research Council. One particular project presently underway involves the evolution and interoperability of the EHR project. The project objectives include the definition of services for remote monitoring and telemedicine and the integration of these applications with EHR, the adaptation of software modules rendering them available as open source components to all stakeholders, among others.
The ultimate aim of such information technology projects is to establish a cohesive system that can support healthcare integration at least on a national level. The water is there to drink. Let us hope the horse takes it in once it reaches there.
PROFILE
Mario Ciampi PhD MSc, studied Computer Engineering at the University of Naples Federico II, Italy and, as a post-graduate, gained a first Master’s degree on Critical Networked Systems in 2007, followed by his PhD on Information Engineering in 2011, both from the University of Naples Parthenope. Since 2004, Dr Ciampi has worked at the National Research Council of Italy (CNR) and is currently a technologist at the CNR’s Naples branch of the Institute of High Performance Computing and Networking (ICAR). He is involved in national projects for the development of interoperability infrastructures for EHR systems. Dr Ciampi also serves on the editorial boards and programme committees of several international journals, conferences and workshops, and is a member of iHealth lab, AMICO, HL7 Italia and @ITIM.
18.03.2013