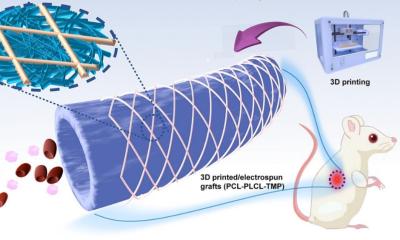
New generation drug-eluting stents
Associated with lower rates of mortality and restenosis than bare metal stents. New 'real-world' reassuring data from the SCAAR registry
A registry -which includes every patient in Sweden having percutaneous coronary intervention (PCI) for the treatment of acute and stable coronary artery disease- has found that PCI implantations using a new generation of drug-eluting stents is associated with lower rates of relapse (restenosis), stent thrombosis and subsequent mortality than older generation drug-eluting stents and bare-metal stents.

The findings, from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR), reported in the European Heart Journal, represent the outcome of treatment in a large "real-world population", and were derived from an analysis of 94,384 consecutive stent implantations performed in Sweden between November 2006 and October 2010.(1)
An earlier study from the SCAAR registry, evaluating stent implantations between 2003 and 2004, had dramatically shown that those treated with drug-eluting stents (DES) had a higher rate of later mortality than those receiving bare-metal stents (BMS).(2)
The results caused uproar, and prompted an immediate decline in the use of DES and an urgent review of their safety. However, follow-up of the same patient cohort two years later (with data extended to 2006) found no increased risk of death between the two groups.(3) The difference in outcome was largely explained by improvements in cardiology practice (including the application of dual antiplatelet therapy after PCI) and the introduction of improved devices.
Conclusions in this latest report, from what is the world's largest PCI registry with the longest follow-up of data, now confirm that mortality rates associated with both the new and old generations of DES were significantly lower than found with BMS. The risk of death was 28% lower with the old generation DES and 45% lower with the new generation; moreover, the new generation DES were associated with a 23% lower mortality rate at two years than the old generation DES.
The authors note that this is the first time any mortality reduction has been shown between DES and BMS, either in randomised trials or in reports from the SCAAR registry itself.
The study also found that the new generation of DES was associated with a 38% lower risk of restenosis and a 43% lower risk of stent thrombosis within two years of implantation than BMS. Late stent thrombosis has been a recurring safety concern with the original DES; the authors suggest that the new generation DES, with "thin, more biocompatible polymers" and greater flexibility, may have contributed to lowering this thrombotic risk.
Speaking on behalf of the SCAAR investigators, cardiologist Dr Stefan James from Uppsala University Hospital in Sweden described the latest findings as "intriguing" - not just because of the lower rates of restenosis with the latest generation of DES, which were expected, but also of stent thrombosis and mortality. "The low rates of restenosis and stent thrombosis correspond with the results of several recent randomised trials," said Dr James, "and this may well translate into mortality reduction in a sufficiently large study population."
However, he warned that all observational data should be interpreted with caution. "Despite the use of appropriate statistical methods," he said, "there may be residual confounding because of differences in concealed baseline variables." Nevertheless, this SCAAR analysis included only patients who where treated after 2006, to ensure that both the older and newer generation DES were used. "Since 2006 no major changes in recommendations for antithrombotic strategies or duration of dual antiplatelet therapy have occurred in Sweden," said Dr James, "so it seems likely that our more favourable outcomes are true findings."
The investigators say their results now add further weight to the strong recommendation for the use of DES as a default strategy in patients expected to tolerate extended dual antiplatelet therapy, in the treatment of coronary artery disease. "But our results also reinforce the need for randomised trials to evaluate the optimal strategy and duration of antithrombotic therapy following PCI in various indications," said Dr James.
#####
1. Sarno G, Lagerqvist B, Frober O, et al. Lower risk of stent thrombosis and restenosis with unrestricted use of ‘new-generation’ drug-eluting stents: a report from the nationwide Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Eur Heart J 2012; doi:10.1093/eurheartj/ehr479
2. Lagerqvist B, James SK, Stenestrand U, et al. Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med 2007; 356: 1009-1019.
3. James SK, Stenestrand U, Lindback J, et al. Long-term safety and efficacy of drug-eluting versus bare-metal stents in Sweden. N Engl J Med 2009; 360: 1933-1945.
* Drug-eluting stents are metallic mesh tubes which keep open narrowed coronary arteries while slowly releasing a medication to prevent the build-up of scar tissue inside the stent.
* The European Heart Journal is the flagship journal of the European Society of Cardiology. It is published on behalf of the ESC by Oxford Journals, a division of Oxford University Press. Please acknowledge the journal as a source in any articles.
09.01.2012