Minimally invasive stents show some advantages over bypass
Compared to open bypass, stenting keeps circulation flowing longer in some patients, small study concludes.

New Johns Hopkins research suggests that people who undergo minimally invasive placement of stents to open clogged leg arteries are significantly less likely than those who have conventional bypass surgery to need a second treatment for the condition within two years.
For now, bypass surgery remains the gold standard for treating symptoms of peripheral artery disease (PAD), but the Johns Hopkins researchers are hopeful that further study will confirm the advantage their study shows for the stents.
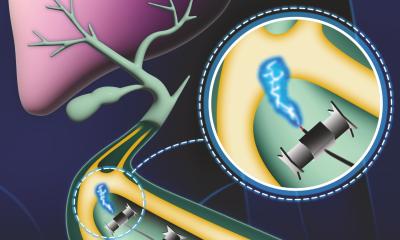
The researchers, reporting online in the Journal of Vascular Surgery, also found that both treatments were equally successful in restoring healthy blood circulation to the legs. But threading a stent through an artery through access in the groin and into the blocked leg vessel to create a wider path for blood requires no general anesthesia and is typically associated with shorter hospital stays and recovery times than open bypass, they add.
“We are constantly looking for the best way to improve quality of life for the 10 percent of the population who suffer from peripheral artery disease,” says study leader Mahmoud B. Malas, M.D., M.H.S., an associate professor of surgery at the Johns Hopkins University School of Medicine, director of endovascular surgery and director of The Vascular and Endovascular Clinical Research Center at Johns Hopkins Bayview Medical Center. “Our study suggests the minimally invasive approach shows real promise, and we are embarking on a large, randomized study of the two procedures to develop guidelines that can be used for determining when a stent is likely to be best and when a bypass cannot be avoided.”
PAD is a common circulatory problem in which narrowed arteries reduce blood flow to the limbs, a likely sign of a widespread accumulation of fatty deposits in the coronary and cerebral vessels, where blockages may lead to heart attacks and stroke, respectively. Without enough oxygen-rich blood flow to keep up with demand, people experience PAD’s most notable symptom — leg pain when walking. As the disease progresses, patients may develop gangrene or open sores that threaten the limb.
Once the pain is serious and chronic, even without walking, doctors consider manually bypassing the blockages. In contrast to minimally invasive stenting, a so-called femoral-popliteal bypass requires a large incision to open the leg, and the surgical attachment of a piece of vein or a synthetic tube above and below the blockage to reroute blood flow.
The small study, just published, was conducted by analyzing records from 104 patients with PAD who either got a stent or a bypass operation at Johns Hopkins Bayview Medical Center between September 2005 and September 2010. The average age of patients in the study was 68 years.
Patients who received stents had a 31 percent risk of needing another procedure to restore blood flow within 24 months, while those who received a bypass had a 54 percent chance of needing another intervention. The researchers found that women were twice as likely as men to need a second operation.
Malas cautions that patients in the stent group may have had better outcomes because 77 percent of them had what were considered smaller blockages, while 73 percent of those who had bypass surgery had larger ones. Physicians use a somewhat subjective measure to choice a treatment, confounding efforts to tease out clear guidelines about when to use stents or bypass.
It is most difficult to determine which course of action to take with medium-sized blockages, Malas says, noting that in his study, patients with longer blockages were more likely to have had a stent in the past that failed, so their diseases may have progressed further along.
Malas says he tells his patients how important it is to adopt healthy habits — exercising, eating properly, taking aspirin and medications to control elevated cholesterol and not smoking — to try to reduce the effects of PAD, which is a “cousin” of coronary artery disease. By the time they need surgical intervention, he says, their disease could not only be threatening their limbs, but their lives.
“We try to improve their quality of life, but stents and bypass won’t cure the patient of PAD at this stage,” he says. “We’re improving circulation, but the disease is still there and it will continue to progress, so modifying other risk factors is a must.”
Other Johns Hopkins researchers involved in the study include Ngozi Enwerem, M.B.B.S.; Umair Qazi, M.D., M.P.H.; Brendan Brown, M.P.H.; Eric B. Schneider, Ph.D.; Thomas Reifsnyder, M.D.; Julie A. Freischlag, M.D.; and Bruce A. Perler, M.D.
For more information:
06.08.2013