Study
Jet air and warm air driers unsuitable for use in healthcare settings
A new study concludes that jet air and warm air hand driers have a greater potential to contaminate washrooms by spreading bacteria into the air and onto users and bystanders. The findings have significant implications for infection control health professionals and purchasing managers responsible for equipping hospital washrooms.
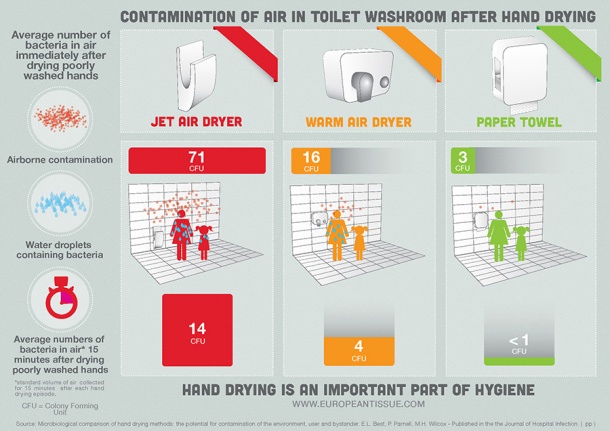

Designed and led by expert medical microbiologist Professor Mark Wilcox, of University of Leeds and Leeds Teaching Hospitals, and funded by ETS the study compared the propensity of three commonly used methods of hand drying to aerosolise bacteria. Jet air driers were found to disperse more bacteria-carrying droplets and spread them further than either warm air driers or paper towels. In addition, bacteria were found to persist in the washroom air for a considerably longer time after the jet air drier stopped.
Airborne dissemination
In carrying out the study, gloved hands were contaminated with a harmless strain of Lactobacillus, an organism not normally found in washrooms. This was done to mimic the bacterial burden on poorly washed hands. Subsequent detection of Lactobacillus in the air proved that it must have come from the hands during drying. Researchers measured the air around the driers and also at distances of one and two metres away. Bacterial counts in the air close to jet air driers were found to be 4.5 times higher than around warm air driers and 27 times higher compared with using paper towels. Next to the driers, bacteria persisted in the air well beyond the 15 second hand drying time, with approximately half (48%) of the Lactobacilli collected more than 5 minutes after drying ceased. Lactobacilli were still detected in the air 15 minutes after hand drying (20% of the total recovered lactobacilli for the jet air drier).
Microbial cross contamination
“It is not acceptable to have contaminated air in washrooms,” said Marc Van Ranst, professor in virology and chairman of the Department of Microbiology and Immunology at the University of Leuven in Belgium. “In hospitals where both medical staff and the general public share facilities, we need to be confident that equipment minimises the spread of infection in order to avoid cross contamination to the wider hospital environment.”
Containment of infection in a hospital setting continually hits the headlines across Europe and is a priority for governments and the medical community. The extent to which jet air driers dispel microbes in the washroom environment raises serious questions concerning policy guidance to avoid the spread of infection in hospitals and other public environments. The data clearly show that hand drying with single use towels contributes least to airborne contamination and hence offers the most hygienic solution. Professor Wilcox commented: "We increasingly emphasise the need to wash hands to control the spread of infection, but we have not considered the best way to dry them. Best does not solely mean convenience. Drying hands using electric driers risks spreading microbes in the washroom, and this is clearly not desirable when trying to limit the spread of bacteria or viruses from person to person."
Dry hands are hygienic hands
“The importance of hand washing to prevent spread of infection is widely accepted. However, to date hand drying has received much less attention," commented Roberto Berardi of the European Tissue Symposium (ETS) who commissioned the study. "Correct hand drying completes the hand washing process and reduces the risk of microbial transmission. Hand drying alternatives in public washrooms are based on either water absorption (single use paper and textile towels) or water dispersal (warm air driers, high speed air driers). This research adds to the existing body of evidence demonstrating that hand drying using towels is associated with lower numbers of microbes both on the hands and in the washroom environment (air) than with warm air or jet air driers," he concludes.
[1]: Microbiological comparison of hand drying methods: the potential for contamination of the environment, user and bystander. E.L. Best,1 P. Parnell,1 M.H. Wilcox 1,2 – Microbiology Department, Old Medical School, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust1 & University of Leeds,2 Leeds LS1 3EX, UK.
Source: Press Release European Tissue Symposium
20.11.2014