Doctors often ignore electronic drug safety alerts
When prescribing drugs electronically, US clinicians often over-ride automatic drug warning alerts in computer-based systems, according to a new study led by researchers at the Dana-Farber Cancer Institute and Beth Israel Deaconess Medical Centre (BIDMC), Boston, published in the Archives of Internal Medicine (9/2/09).
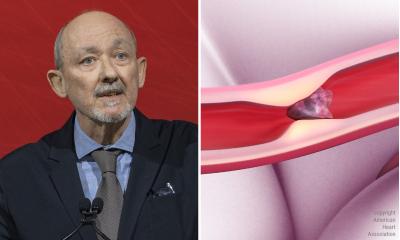
The study suggests that most clinicians find medication alerts a ‘nuisance’ rather than important. ‘Electronic prescribing clearly will improve medication safety, but its full benefit will not be realised without the development and integration of high-quality decision support systems to help clinicians better manage medication safety alerts,’ concludes the senior author of the study, Saul Weingart MD PhD, Vice President for patient safety at the Dana-Farber Cancer Institute and an internist at BIDMC.
For the study, the researchers reviewed the electronic prescriptions and associated medication safety alerts generated by 2,872 clinicians at community-based out-patient practices in Massachusetts, New Jersey, and Pennsylvania. In 2006, the clinicians had submitted 3.5 million electronic prescriptions from January to September inclusive. About 6.6% (one in 15 prescriptions) produced an alert for a drug interaction or a drug allergy. About 98.6% of the 233,537 alerts were for a potential interaction with a drug already taken by the patient.
More than 90% of the drug interaction alerts and 77% of the drug allergy alerts were over-ridden by the clinicians, who typically dismissed even drug interaction alerts rated of high severity, for medications frequently used in combination to treat specific illnesses. They were also less likely to accept an alert if a patient had been prescribed the medication previously.
The study’s first author, Thomas Isaac MD, of BIDMC and Dana-Farber, pointed out: ‘The sheer volume of alerts generated by electronic prescribing systems stands to limit the safety benefits. Too many alerts are generated for unlikely events, which could lead to alert fatigue. Better decision support programmes will generate more pertinent alerts, making electronic prescribing more effective and safer.’
Recommendations: ‘We need to find a way to help clinicians to separate the proverbial wheat from the chaff,’ said Dr Weingart. ‘Until then, electronic prescribing systems stand to fall far short of their promise to enhance patient safety and to generate greater efficiencies and cost savings.’
The researchers recommend improvements for medication safety alerts – including the reclassification of severity of alerts, particularly those often over-ridden; inclusion of an option for clinicians to suppress alerts for medications already received by a patient, and customisation of alerts for a clinician’s specialty.
* A list of potentially dangerous drug interactions identified by the researchers is available at www.dana-farber.org/electronic-medication-safety).
01.03.2009