Point-of-care
Creating a new standard for emergency care
Point-of-care (POC) ultrasound is now commonly used in emergency departments throughout the UK. These instruments provide valuable insight for the assessment of both trauma and non-trauma patients, as well as helping to guide procedures. But for many departments, the use of POC ultrasound is limited by a lack of training and poor instrument availability. Professor Bob Jarman, Consultant in Emergency Medicine at the Great North Trauma and Emergency Centre, discusses the potential benefits of routine ultrasound use and a multisystem approach.
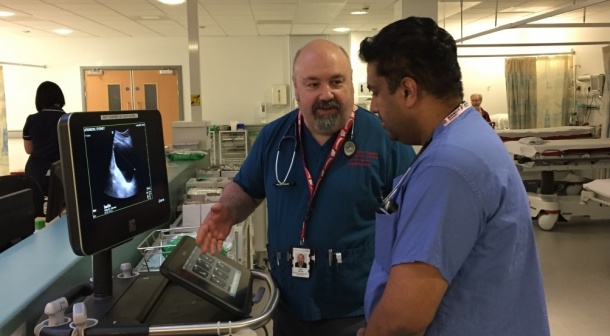

The four key ultrasound skills that a doctor training in emergency medicine in the UK is required to learn are FAST scanning, aortic aneurysm screening, basic echocardiography and venous access. These are the day-in, day-out procedures performed up and down the country but, because there is a lot of interest in ultrasound within our department, we do much more. For example, we regularly undertake more advanced echocardiography, perform thoracic scans, look for abdominal problems, etc. The list of applications for POC ultrasound in an emergency setting is endless – it’s only limited by having a clinical question to ask. As a major trauma centre – the biggest in the north of England – we have increasingly made ultrasound part of our culture here, ensuring that it becomes a routine part of our approach to assessing patients coming into the department.
We are particularly keen on breaking down the major barriers to ultrasound use; a lack of equipment, insufficient access and the misconception that POC ultrasound is trying to replace the radiologist. Fortunately, a lot of work has been done over the past few years to help people understand that ultrasound is an adjunct to our clinical assessment. We are more focused in our use than traditional sonographers; it’s a tool, rather than a standalone investigation, and there’s increasing evidence to show how much more sensitive and specific it is for particular applications.
We are now addressing the other issues – insufficient access to both training and equipment – and have embarked on a long-term programme to demonstrate the benefits of ultrasound to emergency medicine. Thanks to the generous support of FUJIFILM SonoSite, we currently have eight POC ultrasound systems in the department. We have two X-Portes as our main, high-end ultrasound instruments – which have designated locations at opposite ends of the department – and two cart-mounted S-FAST systems, which are our roaming vascular access machines. The remaining four systems are S-FASTs mounted on ‘pendants’ in the resus room, so that they’re readily available to turn on and use, without having to bring a trolley into an already busy space.
When we began this project, we put a lot of thought into how we planned to use the systems, as well as where to locate them throughout the department to maximise their use. The next step was to ensure that staff were sufficiently trained, not just to be competent in ultrasound use, but comfortable and familiar enough with the systems to use them routinely. As a major teaching hospital, we already had many of these training structures in place for junior doctors, but introducing ultrasound use much earlier in their clinical education has been very well received. Medicine isn’t black and white, so having ultrasound to see what’s really going on is one of the key things we’re trying to encourage.
Increasing system availability has also been key to opening up ultrasound use to allied healthcare professionals, including nurses and paramedics. For example, many of our nurses are now training in basic practices, such as bladder volume scanning and vascular access. Although straightforward, these procedures have made a real difference to our productivity, as they are performed in huge numbers. Difficult venous access, for example, might previously have taken up to 45 minutes, occupying a lot of clinician time and requiring multiple attempts. This was upsetting for patients and extremely frustrating for already busy doctors. Now, as soon as we anticipate that there might be a problem, we use ultrasound guidance, and you can cannulate in five to ten minutes for even the most complex cases. Patients love it because it improves the thoroughness of their care and avoids multiple needle-sticks, and staff love it because it makes their lives easier and helps to make the department more efficient.
Developing an interest in ultrasound among junior doctors – even though they don’t usually learn ultrasound skills until later in their careers – is vital. These are the people who will shape medical practice for the next 20 years, so we need to demonstrate the possibilities of ultrasound, and for most it’s a real eye-opener. It’s a work in progress, but getting the junior doctors and even medical students on board is what will drive this forward. Ultrasound is really revolutionising the patient experience and the time it takes to deliver appropriate care, and it’s only by having rapid, widespread access to systems that we can provide this level of service.
Source: FUJIFILM SonoSite
01.05.2017





