Article • Ein aktueller Versuch
Could telemedicine cure Germany’s health system?
The term telemedicine has been around since the 1980s. Ten years later Deutsche Telekom demonstrated the first applications designed to provide medical services to people living remotely such as (based on American ideas) astronauts in space, workers on oilrigs or injured personnel in field hospitals.
Report: Anja Behringer
Since then, the concept of medical care across long distances via telecommunication (Article in german) has not changed. The advantages of fast intervention, diagnostic safety through simultaneous expert opinion obtained via videoconference and ultimately, the associated cost savings still apply – but implementation of the good intentions has been thin on the ground.
A low degree of digitisation
The reason is the lack of digitisation in the healthcare sector, as confirmed by a study commissioned by the Federal Ministry of Economics and Technology last year. The German Federal Association of the Digital Economy believes the most significant reasons why the healthcare sector is lagging behind to be political: rigid legal provisions (around the ban on remote treatment, for instance); rigid structures in statutory health insurance; inertia and the preservation of self-serving interests within the self-governing committees of health insurers and doctors; data protection regulations that are too complex, and a lack of information about the advantages of digital technology provided by the key players in healthcare.
At congresses and workshops examples of best practice are conjured up to learn from other sectors that are much more digitised. One example is lean management, as seen in the automotive industry: streamlined process chains lead to shorter waiting times, reduced distances and handing over of error-free results step by step of the process (‘zero-error principle’). One attempt at improving processes in hospitals with this principle is the use of digital wristbands. In a model project in Berlin the location of hospital patients is monitored through those wristbands to relieve staff and make processes more efficient.
Model project telemedical networking

The model project TELnet@NRW managed by the University Hospital RWTH Aachen follows a different approach. The objective is the development and evaluation of a comprehensive telemedical network as a new digital care platform. The project is funded with €20 million from a Federal Joint Committee innovation fund and focuses on intensive care medicine. More than 20,000 patients have already participated since the start of the intervention phase in October last year. ‘We didn’t really count on that many study patients in the first few weeks! We’re very pleased,’ says Professor Gernot Marx, Director of the Aachen Clinic for Surgical Intensive Care Medicine and Intermediate Care, member of the ZTG-Forum Telemedicine and head of the TELnet@NRW project. ‘We are therefore grateful to all participating project partners, hospitals and networks of surgeries to whom we can attribute the success and who deliver vital data for this project.’
An anticipated 40,000 in- and out-patients are being recruited from 21 participating institutions to obtain valid results. The focus will be on patients with infection-related problems and intensive care patients. A specially created telematics infrastructure facilitates regular tele-intensive, virtual ward rounds by experts from the centres for telemedicine at Aachen and Muenster universities, as well as from partners at the participating hospitals and networks of surgeries. When the project is completed at the beginning of 2020 it remains to be seen whether the results confirm care optimisation and whether telemedical ward rounds should become part of standard medical care.
Switzerland permits ‘remote treatment’
The maxim here is still that the first contact between a patient and treatment provider must be personal
Gernot Marx
Telemedical treatment in Switzerland has been allowed for the last 14 years. Doctors are available around the clock in designated centres and the experiences have been positive, not even to mention the healthcare cost savings of around 17%. Germany is still way behind. ‘The maxim here is still that the first contact between a patient and treatment provider must be personal,’ Marx explains. To ensure these specifications are met, a secure video communication link with fast and protected data exchange between the participating organisations is inevitable.
In practice, the Aachen model project transports digital devices, such as computers, monitors and cameras, to a patient’s bedside or treatment table so that doctors from different hospitals can discuss the best treatment options via a videoconference. The devices also facilitate the transmission of a patient’s X-rays and results. ‘The connection with telemedicine centres at Aachen and Muenster university hospitals is established via highly secured data cables and is therefore well protected,’ the expert explains. Professor Thomas Jäschke at the Institute for Health Care Security and Data Privacy (ISDSG) is the external expert for data protection and IT security who advises the project.
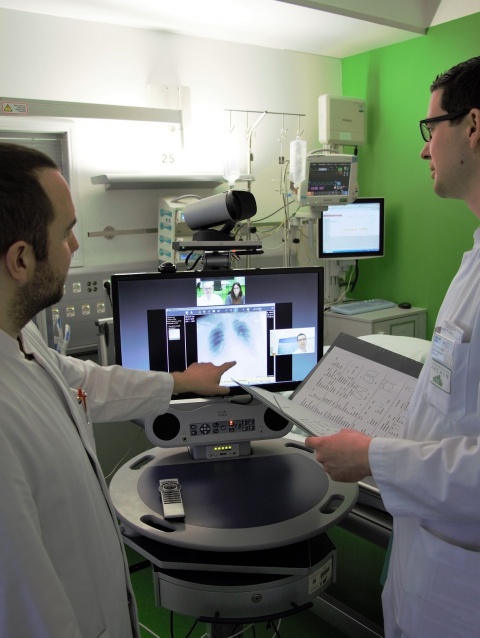
Currently there are regular exchanges about infection-related problems between doctors in private and general practitioner (GP) surgeries and specialists in infectious diseases at Aachen and Muenster university hospitals. There are daily tele-intensive ward rounds, handovers and case conferences. ‘Only around 300 specialists in infectious diseases work in hospitals nationwide,’ Marx points out; not enough to provide comprehensive, personal care. TELnet@NRW is to bridge this gap ‘because early and joint diagnosis is better and ensures adherence to guidelines’. Professor Alexander Zarbock, Director of the Clinic for Anaesthesiology, Surgical Intensive Care Medicine and Pain Therapy at Muenster University Hospital is particularly pleased about cooperation between the hospitals: ‘By making scientific expertise available to colleagues at any time we support the best possible, close-to-home patient care.’
Next to Aachen and Muenster university hospitals, a further 17 hospitals within the Aachen and Muenster regions are also in the consortium, along with the Techniker Krankenkasse (Technical Health Insurance) and the medical networks Gesundheitsnetz Köln-Süd (GKS), and MuM – Medizin und Mehr. The consortium is supported by partnerships with the hospital association North Rhine-Westphalia, the Medical Associations North-Rhine and Westphalia-Lippe as well as all statutory medical insurers in North Rhine-Westphalia. The University of Bielefeld and the Centre provide scientific guidance for Telematics and Telemedicine GmbH (ZTG) in Bochum. The evaluation phases will run to three years.
The data collection method via cluster randomisation and a stepped wedge design allows the project team to compare each hospital with itself and other hospitals over time. Together with continuous data collection this facilitates calculation of the causalities between changes in therapy and diagnosis and the telemedical intervention. After this evaluation a decision will be taken as to whether telemedical ward rounds can become part of standard medical care.
Profile:
Professor Gernot Marx MD, Director of the Clinic for Surgical Intensive Care Medicine and Intermediate Care at the RWTH Aachen, Germany, and member of the ZTG-Forum Telemedicine and Head of the TELnet@NRW project, studied medicine (1987-1994) at Hanover Medical School (MHH), Germany, where he also wrote his doctoral thesis in 1995 and habilitation in 2000. In 2004 MHH appointed him as extraordinary professor and, in the same year, he was awarded a C3-professorship for life for Anaesthesiology, Intensive and Emergency Medicine at the Friedrich-Schiller University, Jena, Germany. In 2008 he was awarded a W-3 professorship for life for Anaesthesiology with a focus on Surgical Intensive Care Medicine and Intermediate Care at Aachen University Hospital. His current focus is on the comprehensive introduction of telematics into healthcare, with a view to implementation as standard care.
05.03.2018