A non-invasive measurement of arterial wall atherosclerosis
By Thaddeus Chodakauskas BS RDMS and Steve Feinstein MD FACC
Non-invasive ultrasound imaging techniques continue to provide a major role in diagnosis and management of patients with cardiovascular disease. The early presence of atherosclerosis predates major clinical events such as myocardial infarction and stroke. Over the last 17 years, the ultrasound-based measurement of carotid artery intima-media thickness (c-IMT) has become a standard for assessing arteriosclerosis and is recommended by the American Heart Association for the non-invasive assessment of cardiovascular risk.
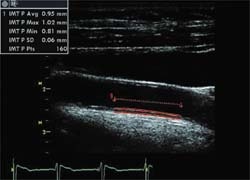
Carotid intima-media thickness is defined as the distance between the lumen-intima interface and the media-adventitia interface, which corresponds to the inner and outer echogenic lines seen on the B-mode ultrasound image. (Fig.1). Measurement of c-IMT is traditionally performed with the image of the carotid artery in the longitudinal axis, revealing the common carotid artery, the carotid bifurcation, and the internal and external carotid arteries. Although these measurements have been performed for years, significant variability exists when measuring the near wall due to technical and acoustic difficulties encountered when imaging the c-IMT of the near wall.
Due to those technical limitations, clinical measurement of c-IMT using B-mode ultrasound is often applied to the far (posterior) wall of the common carotid artery. With the development of non-invasive imaging technologies, ultrasound methods can be used to reliably measure intima-media thickness (IMT). This measurement serves a non-invasive marker of arterial wall atherosclerotic disease. Studies have found that, on average, based on gender and age, the intima-media thickness will increase 0.01-0.03mm per year. (See tables on historical clinical studies of c-IMT).
Intima-media
To perform these studies, radiographers/clinicians use high frequency (7, 10 or 12) MHz linear array transducers with the Vivid 7 Dimension and the Vivid i to efficiently acquire multiple c-IMT measurements within seconds. The semi-automated measurement for intima-media wall is simple, easy and takes less than four steps. The physician receives immediate results, which consist of these parameters: maximum, mean, average and number of data points examined. Using the software application, the c-IMT measurement can be exported directly to a worksheet and report page and, subsequently, placed in the patient’s medical record.
Imaging common carotid artery
• Maximise the depth selection and optimise the gain settings to visualise the posterior intima-media wall of the common carotid artery.
• Attempt to capture the common carotid artery with the jugular vein to improve visualisation of the anterior and posterior carotid walls.
Measuring c-IMT
• Identify a single frame during the end-diastolic phase between the P and Q wave off the ECG trace.
• Approximately 50-60 data points is an adequate sample when used to measure the intima-media thickness.
Performing IMT measurement on the Vivid 7 and Vivid i:
• Select Measurement key on the keyboard.
• Select from the measurement menu carotid folder, then CCA IMT, to identify the right or left carotid artery, then CCA IMT Post, for posterior wall.
• Position the IMT cursor above the intimated wall, then press select key to anchor the first cursor. Reposition the second cursor using the trackball then press select key to anchor the second cursor.
If the IMT measurement result is acceptable, select ‘Transfer’ in the measurement Carotid folder. The results will be displayed in the worksheet and in the final report.
The automated IMT package from Vivid 7/Vivid i: the benefits
• The measurement procedure is not operator dependent and not as time intensive compared with manual IMT measurements.
• The semi-automated technique simplifies the time taken to perform the measurement compared with manual measurement.
• The improved technology enhances c-IMT precision measurements and increases consistency and reliability of the results.
• The methodology is robust, reproducible and builds confidence among radiographers and physicians.
01.09.2007