What makes bedsores tick?
By Friedhelm J Baisch PhD (med. Eng.) of the Institute for Aerospace Medicine*, Cologne, Germany
According to a study by the German Aerospace Centre, bedsores are mainly induced by a combination of gravity and immobility. Gravity exerts skin pressure and tissue shearing stress, which in turn provoke pathological changes if patient mobility is not encouraged.
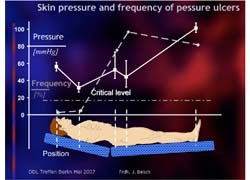
Fig. 1 Pressure level (continuous white line) in regions at risk for bedsores (occiput, shoulder blades, coccyx, ischium and heels). It has been shown that bedsores always develop around the coccyx and ischium, even though the pressure exerted on these regions is not particularly high. However this pressure does exceed the critical threshold (gray dot-dash line). On other hand, it is curious that bedsores do not always develop on the heels, where the highest pressure values occur. Moreover, by rights bedsores should be as prevalent on the occiput as in the coccyx region, since the surface pressure there is nearly the same as in the gluteal region. The critical threshold for surface pressure in this region is slightly under 20 mmHG, which is based on the pressure collapse values for older, cachectic patients in a reduced hydration state. This level is age dependent, and varies inter-individually and according to body region.
Non-invasive, in vivo detection of intra-tissue pressure and tension
Previous calculations regarding the pathological effects of pressure on biological tissue were realised in animal models. Such investigations gave rise to findings such as the Kosiak postulates, which were extrapolated from investigations of tissue pathologies. These postulates allowed investigators, for the first time, to measure stress on human soft tissue using a non-invasive self-constructed pressure stamp and, at the same time, to observe and document the physiological processes in the terminal vessels of the skin and musculature non-invasively.
In this process, erythrocyte movement in the capillary bed was measured in the force direction of the pressure stamp using a Doppler laser, while at the same time the erythrocytes were counted and the oxygen load was measured using a white light spectrometer.
In the gluteal region, the pressure stamp was pointed directly at the ischium. The force was then increased in defined increments until erythrocyte movement ceased in the tissue under the stamp. Up to 50 Newtons were exerted on the skin, with peak pressure ranging as high as 100 mmHG. The deformation was then stepped down using the same increments.
Findings
The force exerted during the various pressure stages was not constant. The force was higher at the beginning of each deformation and then declined to a lower level. The tissue reacted plastically.
The number, oxygen saturation and movement of the erythrocytes decreased as force and deformation lessened. However, substantial numbers of erythrocytes were trapped in the capillary bed when they stopped moving. The oxygen saturation of these erythrocytes was initially high, but decreased as long as the pressure remained constant.
Conclusions
Kosiak’s hyperbola model should be expanded, as this would allow the effects of altered hydration status to be brought into play.
Although tissues tolerate pressure peaks for brief periods, pathologies are provoked by erythrocyte oxygen depletion, i.e. in cases where tissue deformation accompanied by flow stasis remains unchanged for an unduly long period.
The amount of oxygen consumed by maintenance metabolism indicates that tissue deformation is tolerated by nerve tissue for only a few minutes, by skin and inactive musculature by approximately 60 minutes, and by cartilage for several hours. This process of deformation provokes erythrocyte stasis owing to the weight exerted on the surrounding capillary bed.
Kosiak showed that a small amount of pressure can result in a critical weight threshold being crossed, which in turn provokes tissue subsidence if the deformation remains unchanged.
Enlargement of the contact surface via softness does not solve the problem, since softness is habit forming and undermines the patient’s already diminished desire to move autonomously. Hence softness indisputably promotes both immobility and a negative body image. In this respect, it is essential that immobile patients be mobilised several times daily by a nurse, physiotherapist and/or the family caregiver. Only in this way can bedsores be avoided.
The current annual social cost of bedsore treatment is about 0.8 billion euros (2006 figures), which is likely to reach two 2 billion euros in coming years due to increasingly aged populations.
* Institut für Luft- und Raumfahrtmedizin, Deutsches Zentrum für Luft- und Raumfahrt e.v.
Article based on a lecture delivered before the German Bedsore Association (Deutsche Dekubitus Liga) in Berlin in May 2007.
01.07.2008



