New concepts in stroke therapy
Leading neuroradiologist calls for the increased use of catheter and stent procedures
Like a bolt from the blue ischemic stroke strikes a patient unpredictably. The consequences are devastating: stroke is the number one cause of serious disabilities in adulthood - and, in Europe alone, someone suffers a stroke every 20 seconds. Thrombolysis ensures that blood clots in the brain dissolve. However, the majority of patients do not profit from this therapy.

Vascular dilation via catheter appears to be an effective supplement and could be further supported by stenting.
However, although an invasive procedure to treat cardiac infarction has been common for many years, this method is not adequately transferred to ischemic stroke treatment. ‘Why?’ asked Karoline Laarmann, during an interview with Professor Marco Leonardi MD, Head of Neuroradiology at Bellaria Hospital in Bologna, Italy, and President of the European Society of Neuroradiology (ESNR).
Why is the ischemic stroke therapy outcome so poor?
Prof. Leonardi: Time is an important factor. In most cases, the trigger for stroke is a restricted blood flow in the brain. By a thrombolysis the physician administers endovenously an enzyme that dissolves blood clots in the arteries. But for many patients who receive a thrombolysis, the treatment is useless for various reasons.
For example, the patient is hospitalised only after 4 1/2 hours - the time frame in which the thrombolysis
has an effect. Or, a haemorrhage is the trigger for the stroke or cannot be excluded because there is no CT or MR available. In these cases the thrombolysis is also of no use, in fact, it would increase the bleeding. Furthermore, if the vascular occlusion is caused by arteriosclerosis, thrombolysis is only of short-term effectiveness - the vessel
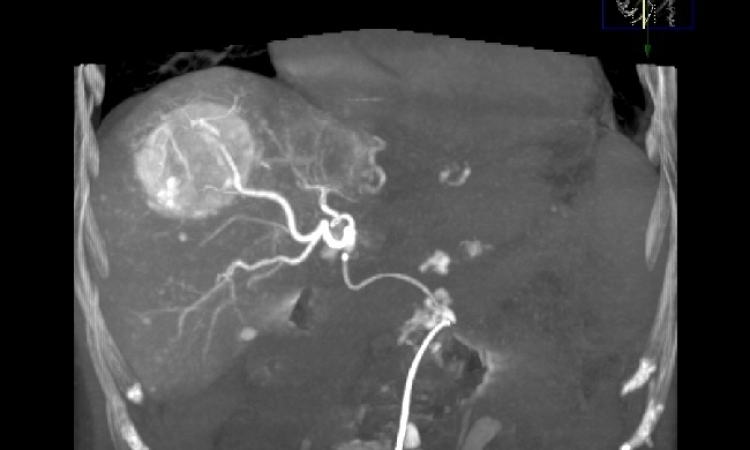
will quickly close again. Therefore, these patients should be additionally treated with vascular dilation or dethrombosis by catheter, in an intra-arterial approach.
Which stroke patients profit from a catheter treatment?
Prof Leonardi: All those who do not respond to endovenous treatment -- such as thrombolysis via endovenous injection -- after an observation of about 30 minutes. Furthermore, intra-arterial catheter treatment is advisable for patients with a large occluded vessel (e.g. carotid siphon, basilar artery). These patient groups can be quickly identified nowadays with MR or CT. Most important is to put vascular diagnosis in the foreground. The causes for ischemic stroke are vascular diseases. Nevertheless, up to now diagnostic efforts have concentrated on the brain itself, while the vessels were neglected.
If there is every indication that re-opening closed arteries is crucial for successful ‘blood clot therapy’, why are stents and catheters still deployed so rarely in stroke treatment?
Prof Leonardi: From the medical point of view there is no reason. We have a power problem here, not a scientific one: unfortunately, neurologists have struggled to cooperate with neuroradiologists for a long time, because it would have put the decision-making in the hands of neuroradiologists instead of neurologists. They argued against the invasive endovascular approach -- that it was not evidencebased. But lately the literature on
this topic, as well as the number of centres in Europe and USA performing the endoarterial procedure is
increasing and so does the understanding of the method. Now neurologists understand they cannot stop progression for much longer, so they have changed their argumentation tactic. Currently, they say they want to do the procedure on their own because we don’t have enough trained neuroradiologists to do the job instead.
But is it appropriate to let neurologists do it?
Prof Leonardi: No, I do not think so. It is difficult to say but I would like to be very clear: Neuroradiology is not an established medical specialty yet (unfortunately) but this is another story. In our world we have many very good neuroradiologists that started their career as neurologists or neurosurgeons and eventually embraced Neuroradiology and became neuroradiologists. Now the approach is different neurologists and neurosurgeons are afraid of loosing part of their field for neuroradiologists, they believe that Interventional Neuroradiology is somehow easy (of course because if the neuroradiologists are able to do that…) but they lack completely the radiological culture that is needed for this work and do not want to learn it, they wont to keep their neurological identity.
So it is very good if a neurologist or a neurosurgeon decide to become neuroradiologist, their clinical culture is extremely important and if they apprehend the radiological side of the discipline they can become a very good neuroradiologist. But it is completely wrong to pretend Interventional Neuroradiology to become Neurology or Neurosurgery.
How did your department of Neuroradiology at Bellaria Hospital in Bologna develop?
Prof Leonardi: It took to me ten years to convince the neurologists of Bologna to start the stroke treatment. Since one year we do thrombolysis with endovenous “general” administration of drugs. We did endoarterial dethrombosis with enzymes or mechanical clot retrieval only in very few cases. Now we are starting a research project for endoarterial dethrombosis with a new device. Stent intracranial is difficult and dangerous, there is the need for highly skilled neuroradiologists and an organization for fast diagnosis and fast angiography which is not yet ready in our hospital it will take some time, because the need of human resources and technological is high and we have enormous financial difficulties. We regularly perform intracranial stenting in aneurysms treatments.
Does stroke treatment in Europe differ?
Prof Leonardi: Yes, it does. There are countries like Denmark, UK, and Switzerland were the organization of stroke diagnosis and therapy is more advanced, In several countries there are Stroke Units organized with a large interdisciplinary team offering fast diagnosis and fast treatment with all the possible approaches. In Italy we have many Stroke Units, organized by neurologist, without an interdisciplinary approach and without the possibility of a full 24h/7d activity. In Bologna we had for many years a neurological Stroke Unit opened from 8 a.m. to 2 p.m.
The organizational problem is the most difficult followed by the need of a different mentality about emergency work, the kind of mentality that neurologist do not understand, because the usual activity of neurologists is far from the emergency room, they deal with difficult diagnosis, difficult pathology , most frequently needing a long work of examination. They are usually not men of action but thinking minds. Neurosurgeons think less and cut more, this is partially a joke, but certainly neurosurgeons have the perfect understanding of what means an emergency problem, as we, neuroradiologists, do too. Medical emergency physicians can also be in this kind of team with very good possibilities.
Please allow me to state that I am not criticizing neurologists or neurosurgeons. I spent all my professional life with them and can say they can be wonderful colleagues, our disciplines are strongly interconnected and we obtain the best results in working together, in a complementary interdisciplinary work, keeping our specificities and in a relationship based on mutual respect.
27.01.2010