Hyperbaric oxygen treatment
Rationale and effectiveness in the non-healing diabetic foot ulcer patient.
By Peter HJ Mueller and Robert A Warriner III

Problem wounds represent a significant and growing challenge to our healthcare systems. The incidence and prevalence of these wounds are increasing in the population resulting in growing utilisation of healthcare resources and budgets expended. Foot ulcers in patients with diabetes contribute to over half of lower extremity amputations in the USA in a group at risk representing only 3% of the population. In response to this challenge specialised programmes have emerged designed to identify and manage these patients, using a variety of new technology to improve outcomes. Hyperbaric oxygen treatment has been increasingly utilised in an adjunctive role in many of these patients coinciding with optimised patient and local wound care.
Hypoxia in Wound Healing Failure
Normal wound healing proceeds through an orderly sequence of steps involving control of contamination and infection, resolution of inflammation, regeneration of the connective tissue matrix, angiogenesis, and resurfacing. Several of these steps are critically dependent upon adequate perfusion and oxygen availability. The end result of this process is sustained restoration of anatomical continuity and functional integrity. Problem or chronic wounds are wounds that have failed to proceed through this orderly sequence of events and have failed to establish a sustained anatomic and functional result. This failure of wound healing is usually the result of one or more local wound or systemic host factors inhibiting the normal tissue response to injury. These factors include persistent infection, malperfusion and hypoxia, cellular failure, and unrelieved pressure or recurrent trauma.
The hypoxic nature of all wounds has been demonstrated, and the hypoxia, when pathologically increased, has correlated with impaired wound healing and increased rates of wound infection. Local oxygen tensions in the vicinity of the wound are approximately half the values observed in normal, non-wounded tissue. The rate at which normal wounds heal has been shown to be oxygen dependent. Fibroblast replication, collagen deposition, angiogenesis, resistance to infection, and intracellular leukocyte bacterial killing are oxygen sensitive responses essential to normal wound healing. However, if the periwound tissue is normally perfused, steep oxygen gradients from the periphery to the hypoxic wound centre support a normal wound healing response.
Measurement of Wound Hypoxia
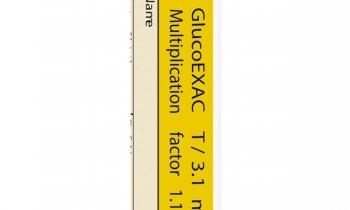
Transcutaneous oxygen tension (PtcO2) measurements provide a direct, quantitative assessment of oxygen availability to the periwound skin and an indirect measurement of periwound microcirculatory blood flow. The application of PtcO2 measurement in the assessment of peripheral vascular disease has been well described by Scheffler and its application to wound healing problems by Sheffield. This technology allows objective determination of the presence and degree of local, periwound hypoxia serving as a screening tool to identify patients at risk for failure of primary wound or amputation flap healing. It can also be used during assessment of patients with lower extremity wounds as a screening tool for occult peripheral arterial occlusive disease.
Physiology of Hyperbaric Oxygenation of Wounds
Regardless of the primary aetiology of problem wounds, a basic pathway to non-healing is the interplay between tissue hypoperfusion, resulting hypoxia, and infection. A large body of evidence exists which demonstrates that intermittent oxygenation of hypoperfused wound beds, a process only achievable in selected patients by exposing them to hyperbaric oxygen treatment, mitigates many of these impediments and sets into motion a cascade of events that leads to wound healing. Hyperbaric oxygenation is achieved when a patient breathes 100% oxygen at an elevated atmospheric pressure. Physiologically, this produces a directly proportional increase in the plasma volume fraction of transported oxygen that is readily available for cellular metabolism. Arterial PO2 elevations to 1500 mmHg or greater are achieved with 2 to 2.5 atm abs with soft tissue and muscle PO2 levels elevated correspondingly. Oxygen diffusion varies in a direct linear relationship to the increased partial pressure of oxygen present in the circulating plasma caused by hyperbaric oxygen therapy. This significant level of hyperoxygenation allows for the reversal of localised tissue hypoxia, which may be secondary to ischaemia or to other local factors within the compromised tissue.
In the hypoxic wound, hyperbaric oxygen therapy acutely corrects the pathophysiology related to oxygen deficiency and impaired wound healing. A key factor in hyperbaric oxygen therapy’s enhancement of the hypoxic wound environment is its ability to establish adequate oxygen availability within the vascularised connective tissue compartment that surrounds the wound. Proper oxygenation of the vascularised connective tissue compartment is crucial to the efficient initiation of the wound repair process and becomes an important rate-limiting factor for the cellular functions associated with several aspects of wound healing. Neutrophils, fibroblasts, macrophages, and osteoclasts are all dependent upon an environment in which oxygen is not deficient in order to carry out their specific inflammatory or repair functions. Two groups of induced responses occur:
1) Improved leukocyte function of bacterial killing, antibiotic potentiation, and enhanced collagen synthesis occur during periods of elevated tissue PO2.
2) Suppression of bacterial toxin synthesis, blunting of systemic inflammatory responses, and prevention of leukocyte activation and adhesion following ischaemic reperfusion are effects that may persist even after completion of hyperbaric oxygen treatment.
In addition, vascular endothelial growth factor (VEGF) release is stimulated and platelet derived growth factor (PDGF) receptor appearance is also induced. The net result of serial hyperbaric oxygen exposures is improved local host immune response, clearance of infection, enhanced tissue growth and angiogenesis with progressive improvement in local tissue oxygenation, and epithelialisation of hypoxic wounds.
Diabetic Lower Extremity Wounds, the Prototype Hypoxic Wound
Lower extremity ulcers and amputations are an increasing problem for people with diabetes. Up to 6 per cent of all hospitalisations for diabetics include a lower extremity ulcer as a discharge diagnosis. When present, an ulcer increased hospital length of stay by an average of 59% compared to diabetics admitted without lower extremity ulcers. Finally, once an amputation occurs, nine to 20% of diabetic patients will experience an ipsilateral or contralateral amputation within 12 months and 28-52% within five years. The cost of care for a new diabetic foot ulcer has been calculated to be $27,987 in the two years following diagnosis.
Management, likewise, has been extensively described and includes careful attention to identification and management of infection, aggressive surgical debridement, evaluation and correction of vascular insufficiency ambulatory off-loading, and glycaemic control. While a full discussion of these interventions is beyond the scope of this review, they form the basis of effective diabetic foot ulcer management and must be applied consistently if adjunctive interventions are to provide an additive value. Other interventions have recently been advocated including topical application of a recombinant human platelet derived growth factor (PDGF-BB, becaplermin), bio-engineered human monolayer fibroblast grafts and bi-layer fibroblast and keratinocyte grafts, and negative pressure wound therapy (wound vac). Clearly, regardless of the interventions applied, limb salvage rates improve when care is applied in a multidisciplinary setting using comprehensive protocols for care.
Local wound hypoxia plays a pivotal role in diabetic wound healing failure and limb loss as evidence by the report by Pecoraro that when periwound PtcO2 values were below 20 mmHg they were associated with a 39 fold increased risk of primary healing failure. While aggressive distal lower extremity bypass grafting and lower extremity angioplasty have contributed to increased wound healing and limb salvage rates, technical grafting success does not necessarily equate with limb salvage. Hyperbaric oxygen treatment offers an intriguing opportunity to maximise oxygen delivery in the setting of minimal or insufficiently corrected blood flow.
Clinical Experience with Hyperbaric Oxygen Treatment in Diabetic Lower Extremity Wounds
Since 1999 there have been eight published independent evidence-based reviews that have addressed the effectiveness of hyperbaric oxygen treatment in problem, chronic wounds. These reviews have evaluated the results of:
1) Four randomised controlled clinical trials of hyperbaric oxygen treatment in diabetic lower extremity wounds.
2) Two randomised controlled trials in non-diabetic leg ulcers or where wound healing was not the outcome indicator.
3) Two non-randomised controlled trials in diabetic lower extremity wounds.
4) One prospective case series of hyperbaric oxygen treatment and infra popliteal angioplasty in diabetic lower extremity wounds
5) Eight prospective or retrospective uncontrolled case series in diabetic lower extremity wounds.
In the controlled trials, 334 patients were included in the hyperbaric oxygen treatment arms and 582 patients in the control arms. In the cases series, 1590 patients were reported. There were additional small retrospective series that were not included in this review.
In general, while specific selection criteria for inclusion for hyperbaric oxygen treatment were not provided, inference from the description of patients included can be made that most were Wagner grade III or greater ulcers since ‘diabetic gangrene’ was frequently mentioned as a descriptor of patients included. Hypoxic transcutaneous PO2 values were not mentioned as an inclusion criterion for selection for the randomised controlled clinical trials.
In summary, the available evidence supports classifying the use of adjunctive in hyperbaric oxygen treatment for diabetic foot ulcers meets the requirements for AHA Class I definitely recommended based on Level A evidence of positive randomised controlled trials with statistically positive results. In the broader category of hypoxic wounds, based on the absence of trials using measured tissue hypoxia as a patient inclusion criterion, adjunctive hyperbaric oxygen treatment meets the requirements for AHA Class IIb acceptable and useful with fair to good evidence for support based upon limited level clinical trial data but with substantial level B non-randomised retrospective case series where PtcO2 values were reported but not used for inclusion, animal models with very reasonable extrapolations from existing data, and rational conjecture and historical acceptance. Randomised clinical trials should be performed to better define a ‘hypoxic’ wound as a unique wound category and the value of hyperbaric oxygen treatment in this setting.
Hyperbaric Oxygen Treatment Protocols
Treatment protocols vary depending on the severity of the problem and the type of hyperbaric chamber used. In larger multiplace chambers, treatments are delivered at 2.0 to 2.5 ATA for 90 to 120 minutes once or twice daily. In monoplace chambers patients are usually treated at 2.0 ATA. Patients with serious infections may require hospitalisation for intravenous antibiotics and better diabetes control. Hyperbaric oxygen treatment in such cases is usually rendered twice daily for 90 minutes. Once stabilised most of these patients can be treated on a once daily basis as outpatients. When infection is controlled, blood flow optimised (wherever possible), other interventions that may hasten tissue growth and wound closure such as negative pressure wound therapy (wound vac), bio-engineered tissue grafts, or surgical reconstruction or closure can be used in combination with adjunctive hyperbaric oxygen treatment to hasten recovery. The October 2000 Office of the Inspector General report to the Department of Health and Human Services identified that active physician oversight of hyperbaric oxygen treatment led to improved outcomes.
Utilisation Review
Hyperbaric oxygen treatments are performed at 2.0 to 2.5 ATA for 90 to 120 minutes of oxygen breathing. The initial treatment schedule is dictated by the severity of the disease process. In the presence of limb-threatening infection after debridement or incompletely corrected peripheral arterial occlusive disease, patients may require twice daily treatments. Once stabilised, treatment frequency may decrease to once daily. Utilisation review is required after the initial 30 days of treatment and at least that frequently thereafter.
Cost Impact
Hyperbaric oxygen therapy as an adjunct to medical and surgical treatment of difficult problem, chronic wounds, particularly diabetic lower extremity wounds, has been shown to be cost effective in limited reviews, especially when compared to major lower extremity amputation. Preventing a below the knee amputation by salvaging a ray resection or transmetatarsal amputation of the foot or preventing an above the knee amputation by preserving a below the knee amputation represents a satisfactory outcome in these high-risk patients. Wounds healed with adjunctive hyperbaric oxygen treatment have also demonstrated excellent durability.
Outlook
Considering the existing evidence, the Jury of the ECHM Consensus Conference on hyperbaric oxygen in the treatment of foot lesion in diabetic patients, held in London (December 1998) stated: ‘There is some evidence from a number of trials, each of which suffers from methodological problems, to support the use of HBO in ischaemic limb-threatening problems in diabetic patients. Patients with diabetic foot problems warrant treatment by foot care teams with careful evaluation of metabolic, neuropathic and vascular factors. Potential candidates for HBO may include those with Wagner grade 3 to 5 lesions treated unsuccessfully by standard methods when amputation seems a possibility.’
A result of the meeting was the recognition of the urgent need for a collaborative international trial for the application of HBO in diabetic foot lesions. This study is now well advanced in Europe as a multi-centric, prospective, controlled, randomised project to evaluate the efficacy of HBO in the healing of foot lesions in diabetic patients. This had been designed by the Working Group 4 of the COST Action B14 (www.oxynet.org), which was co-ordinated by the Research Foundation of the European Commission until March 2005. Results of that study should become available in the near future.
02.08.2006