High quality care at low costs
Whilst participants at the ‘Boundary-less Hospital in Health Care Networks’ conference, organised by the Centre for Advanced Studies in Management (CASiM) at Leipzig Graduate School of Management (HHL) in mid-June agreed on the need as such, there was plenty of room to discuss exactly which changes could make the German healthcare system future-ready.

The health economy, a 100-year-old success story, still has much unused potential, according to Dr Nicolaus Henke, Director Healthcare Systems & Services at McKinsey & Company. He suggested three options to tap this potential: embracing the data opportunities; re-inventing delivery models and leading a multi-sector approach to build healthy 21st century cities.
Wolfgang Bayer, CEO of Siemens Healthcare in Germany, and Dr Ulf M Schneider, chairman of the Management Board of Fresenius Group, explored the growth potential of their companies. Siemens is focusing on companion diagnostics, i.e. further development of approaches in personalised medicine.
In December 2013, Siemens launched a partnership with Pfizer to develop and commercialise lab diagnostic tests designed to help physicians make personalised therapy decisions for their patients. Dr Ulf Schneider explained why Fresenius has been acquiring hospitals since 2001. Only the interaction of medical technology products and their clinical environment, he argued, will generate more value for the company in the long-term, particularly because the industrialised countries spend up to fifty percent of their healthcare budgets for services – much more than for medical technology products.
Dr Sören Eichhorst, physician and head of the McKinsey Hospital Institute, suggested new chains of value creation. ‘In healthcare, value is easy to define: it is that which we optimise every day, namely costs and quality. We all have to make joint efforts to ensure that cost efficiency is directed towards the right treatment,’ emphasised Eichhorst, a former head of a hospital group and today a hospital consultant.
Patients should receive exactly what they need – high quality at low costs, he said… this is not a contradiction but a perfect match: ‘There is a clear trend: the personal experience of the patient and his opinions and perceptions play an increasing role.’ How does the patient perceive the treatment? What is the treatment benefit? To what extent can, and should, a patient influence treatment? Where is the patient as well informed as the physician?
For a long time, Eichhorst reminded the audience, the focus has been on patient output, but the outcome, he emphasised, is equally important. The way hospitals define ‘patient’ is changing and in the future the patient experience will affect reimbursement. The lack of communication between the different professions in a hospital is an enormous obstacle for optimisation, he believes. ‘Ideally, the decision-makers of different hospital departments, such as clinical services, nursing, administration or IT, are at the centre of communication processes. However, the network analyses of hospitals often show that these people do not talk to one another. As far as I’m concerned, further standardisation and ‘professionalisation’ of hospital workflow are desirable. As soon as the actors involved in every step – from admission to discharge – are clearly defined, the individual groups leave their isolation and communication improves.’
The consultant then identified a further trend: the increasing interest of medical technology and pharmaceutical companies in the core area, ‘hospital’. ‘For a manufacturer, it won’t do to simply offer the next CT. His added value is created by understanding hospital processes.’ Today, Eichhorst observed, many companies make efforts to do just that – trying to understand the procedures and identify opportunities to standardise and find ways to make the healthcare system better in terms of quality and costs. Therefore, he adds, ‘projects are being funded that will not yield an immediate profit, but which will help improve future business decisions.’
If the opportunities provided by new technologies are used, a disruptive change might be possible, despite the strict regulation of the healthcare market. In short, he concluded, the future focus should be on a balanced doctor-patient relationship, up-to-date means of communication and innovative hospital concepts.
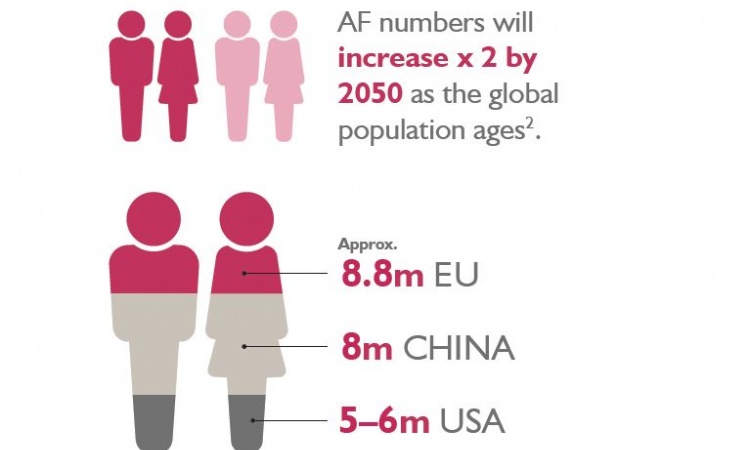
Professor Manfred Dietel, of Charité Berlin, encouraged a broad public discussion on the affordability of the healthcare system. In view of exploding costs of personalised medicine and ageing population, we must ask who will pay those rising costs, he asked, and suggested raising healthcare insurance premiums to avoid having to exclude certain patient groups from medical care in the future.
The Centre for Advanced Studies in Management (CASiM) conference was dedicated to health economy for the first time, reflecting an expanded course to be provided this summer. The two-year part-time MBA programme in General Management will focus on Hospital Management, initially only at Leipzig, and later also at the Cologne campus.
01.08.2014