Doctors’ shifts and patient safety raises concern
Report: Mark Nicholls
The reduction in junior doctors’ hours to 48 hours a week with the introduction of the European Working Time Directive (EWTD) has increased the number of work shifts and continuity of care is suffering as patients are ‘handed over’ again and again to different doctors, according to the Royal College of Physicians (RCP).
After receiving anecdotal reports of problems relating to handover practice, in March this year the RCP launched a survey to seek doctors’ experiences in this respect and lead to initiatives to improve the handover situation for the benefit of all concerned.
The initial results from the 3-week long survey, presented at a meeting in May, revealed examples of good and bad handover practice in British hospitals and also that there was no consistent standard for handovers. The college is now analysing these early results as it moves forward in its efforts to improve handover practice and find solutions.
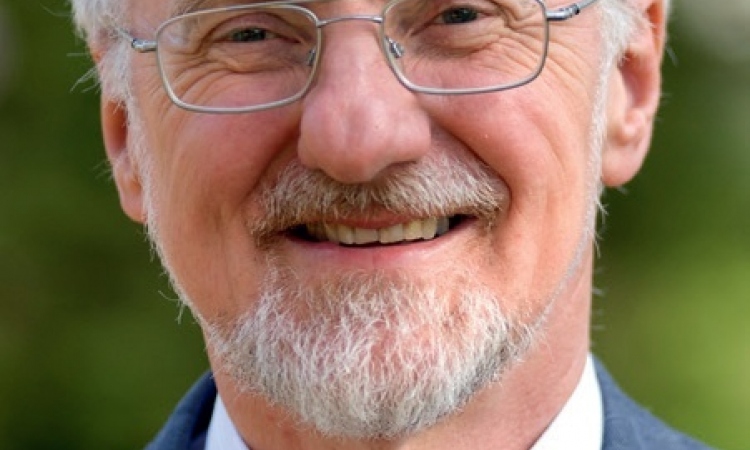
Cardiologist Dr Jean McEwan*, the RCP’s Improving Working Lives Officer and project leader of the handover study, said the aim was to gain three things: to understand what current handover practice is within hospitals; to understand the challenges that doctors feel they face when trying to implement good handover practice, and to gather examples of how pioneers of the work on handover are trying to solve the problem. ‘When trying to assist doctors in implementing good handover we had no clear idea of what is currently in place and the challenges currently faced in trying to implement good handover practice,’ she explained. ‘The survey was necessary to garner this information and to ensure that work by the RCP is as beneficial as it can be for patients and doctors.’
All consultants who participate in the RCP consultant census and all trainees registered with the Joint Royal Colleges Postgraduate Training Board (JRCPTB) – in total 7,417 doctors – were invited to take part.
While acknowledging this represents a subset of all doctors, the RCP believe that opinions gathered in this group are likely to indicate some problems that are universal. In a future stage of the handover project, the college will pursue a multidisciplinary input.
‘We hope the survey will in particular identify whether there are areas where there are no formal arrangements in place for the handover of patients,’ Dr McEwan said, adding: ‘Further to this, we hope that it will highlight the work that needs to be done in order to ensure that handover provides the benefits that it can for patients and doctors alike.’
The RCP believes there will be long term benefits for patients, doctors and hospitals in effectively addressing the issue.
Along with improving patient safety, care and experience of healthcare, Dr McEwan added that good handover is likely to be effective in reducing the length of in-patient stays, as well as possibly providing educational benefit to those who participate in it.
The RCP and partners are now focusing on the survey data to decide what practical work needs to be done to implement best handover practice in hospitals.
*As Improving Working Lives Officer for the RCP’s Medical Workforce Unit, Dr Jean McEwan is involved with areas of gender balance, flexible working and improving the work/life balance within the medical profession.
Based at the Royal Free and University College London Medical School, the UCLH, NHS Foundation Trust and the Heart Hospital, Dr McEwan is a Reader in Cardiology, an Honorary Consultant Cardiologist and Director of Clinical Teaching
07.07.2010