Source: Shutterstock/Elnur
Article • Patient blood management
Blood transfusions: Patient groups should be precisely defined
Although blood transfusion today is a well-established and safe procedure, the medical science community has not yet arrived at a consensus regarding appropriate patient blood management (PBM) methods.
Report: Anja Behringer

‘Many PBM approaches have not yet been scientifically validated; consequently over- as well as under-transfusion might be associated with adverse events and complications for the patient,’ explained Dr Erhard Seifried, Medical Director and Medical Managing Director of the blood donation services of the German Red Cross and professor for transfusion medicine and immunohaematology at Frankfurt/Main University Hospital.
Seifried chaired an international conference in Frankfurt that aimed to clarify the relevance of blood transfusions and establish alternative treatments for anaemia. However, it was impossible to define a set of precise standards. The 200 participating experts from 40 countries and five continents were flabbergasted.
Systematic transfusions
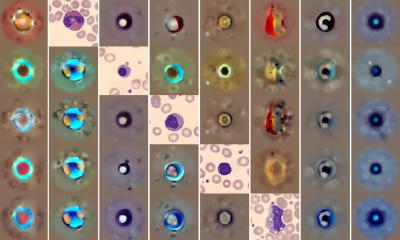
Blood transfusions are needed ad hoc when accidents or surgeries cause severe blood loss or, on a regular basis, for patients suffering inherited blood cell disorders such as sickle cell anaemia or thalassaemia, or cancers such as leukaemia, or myelodysplastic syndrome (MDS). Moreover, external factors e.g. lack of iron or vitamins, radiation for cancer therapy, or certain types of medication, can negatively affect blood cell formation. Appropriate blood management and determining the correct volume of blood to be administered requires complex preparatory exams. However, actual treatment methods vary widely from country to country – this much was ascertained during the ICC-PBM conference (see below for more info).
Professor Dr Reinhard Burger, immunologist and Director of the Robert Koch Institute in Berlin from 2010-15, was somewhat exasperated when speaking with our EH correspondent: ‘Nothing is clear, there are no comprehensive studies and only a small percentage of existing studies can be analysed.’ 1,500 studies were evaluated for the issues addressed by the consensus conference, but a mere 142 met modern evidence standards and could be drawn upon as a basis for discussion. The experts’ idea: to evaluate the data scientifically and objectively determine the best possible treatment for each individual patient. This turned out to be an impossible task.

Blood counts of older and chronically ill patients established prior to surgery often show anomalies, which means more and larger volumes of banked blood are needed. Since pre-operative anaemia is considered a risk factor during surgery associated with increased mortality, myocardial infarction, stroke and kidney diseases, it was suggested that anaemic patients be identified prior to surgery in order to stimulate own blood cell formation. One way to do this is the administration of iron and erythropoietin – known as EPO – or a combination of both.
The advantages and disadvantages of these substances compared to conventional procedures have not yet been scientifically ascertained since such a therapy is not without risks. Intravenous administration of iron can exacerbate infections and cause allergic reactions, while the manufacturers of erythropoietin point out a number of possible adverse events such as thrombosis, as Professor Seifried reported.
Anaemia patients need individual evaluation
After all, we treat the human being, not the haemoglobin concentration
Reinhard Burger
Whilst the analysed studies did not provide sufficient data to clearly correlate preoperative anaemia and complications such as stroke, myocardial infarction and kidney disease, the experts did arrive at a unanimous conclusion: prior to surgery anaemic patients should be identified. However, anaemia treatment must be decided on a case-by-case basis. The experts recommend a decision algorithm that includes factors such as age, co-morbidities, haemoglobin concentration, duration of anaemia and type of surgery. ‘When treating anaemia pre-operatively, each patient needs to be evaluated individually since spontaneous anaemia requires a very different approach than long-term iron deficiency. ‘Moreover, in older patients treatment is more urgent than in younger ones,’ Seifried explained. Thus, the decision to administer iron, erythropoietin or a combination of both, depends on numerous factors.
The experts agreed on a second point. To date there is not a single study on preventive blood transfusions. Consequently, no recommendation can be issued at this point. The ICC-PBM conference, Burger said, did provide pointers and possible new approaches for future studies.
The conference discussions also showed that a low haemoglobin concentration is not a sufficient indicator for treatment. According to the World Health organisation (WHO) anaemia is present with a haemoglobin concentration of <12 g/dl in women and <13 g/dl in men. ‘These values were defined fifty years ago and are based on data from five studies – today this is not conclusive evidence,’ Seifried pointed out. Adding to this, Burger said: ‘Patient groups must be defined more precisely and be viewed in a more differentiated way. After all, we treat the human being, not the haemoglobin concentration.’
Profile:
The President of the Robert Koch Institute, Dr Reinhard Burger, was formerly head of the Department for Immunology as well as the Department for Infectious Diseases. He gained his PhD (1976) and habilitation (1982) at the Institute for Medical Microbiology, Mainz University and, between 1983-87 was professor for immunology at the Faculty for Theoretical Medicine in Heidelberg University, Germany. In 1989, Burger joined the Free University of Berlin (University Hospital Benjamin Franklin) as professor for immunology. He has also been a visiting scientist in the National Institutes of Health in Bethesda, MD, USA, Harvard Medical School, Boston, USA, and the Medical University in Wuhan, China. In 1993 Burger became chairman of the National Advisory Committee on Blood at the German Federal Ministry for Health.
The International Consensus Conference on Patient Blood Management (ICC-PBM) aims for a transparent and scientific approach and international cooperation. This is very much a joint event, supported by the American Association of Blood Banks (AABB), the International Society of Blood Transfusion (ISBT), the German Society of Transfusion Medicine and Immunohaematology (DGTI), the French Society of Blood Transfusion (SFTS), the Società Italiana di Medicina Trasfusionale e Immunoematologia (SIMTI), the European Blood Alliance (EBA) and the Centre of Evidence-Based Practice (CEBaP). ICC-PBM is also supported by the Australian Red Cross Blood Service (ARCBS), Canadian Blood Services (CBS), International Collaboration for Transfusion Medicine Guidelines (ICTMG), International Society on Thrombosis and Haemostasis (ISTH), National Blood Authority (NBA), and the EU Directorate General Health.
19.07.2018