Article • Value-based radiology
We have impact on value!
The movement to Value-Based Healthcare gives no value to diagnostic processes, including Radiology. ESR aims to establish a more holistic approach to help Europe’s single-payer systems shift to a new economic model.
Report: John Brosky
The organisers behind Value-Based Healthcare (VBH) are gaining ground in an effort to transition public and private payers toward value-based reimbursement.To date, the International Consortium for Health Outcomes Measurement (ICHOM) has published 21 sets of standards covering almost half of what it defines as the global disease burden.
Some European health care groups have experimented with this approach with mixed results, notably the Karolinska University Hospital in Sweden.
Radiology adds impact, more than what is being called value, which is only a calculation of outcome versus cost. It’s not easy to value the impact of diagnosis.
Professor Lorenzo Derchi
VBH started in the United States as a response to ineffective models introduced by payers to manage costs of healthcare services, such as fee-for-service or capitated payment approaches. Incredibly, VBH does not include diagnostic processes, focusing instead on therapeutic outcomes. Value is defined by treatment without considering the multi-disciplinary evaluation of the patient that in the first instance determines the patient’s pathway for care.
‘It’s still early days,’ said Professor Lorenzo Derchi, who is chair of the Value-Based Imaging Working Group of the European Society of Radiology (ESR) and the ESR’s First Vice-President. ‘Value-Based Healthcare is an economic approach that is interesting, but not the only possible approach. The initiators of this movement come from the Harvard School of Economics, not the medical school,’ he told European Hospital during our recent interview. ‘It does not consider the whole spectrum of care, a holistic approach to the patient. With this model, radiology is not considered for its role in providing guidance for the therapy, nor for following up the treatment to fine-tune and adapt that treatment.
‘Radiology adds impact, more than what is being called value, which is only a calculation of outcome versus cost. It’s not easy to value the impact of diagnosis,’ he pointed out. ‘It becomes easier for calculations if the diagnosis is taken for granted. It’s not clear if ICHOM did not consider diagnostics, or if they considered it but found it too difficult to measure as a value.’
In September the ESR published a Concept Paper On Value-Based Radiology in the Society’s journal, Insights into Imaging, seeking to contribute to the discussion on this critical issue and to move it to the next level by asserting that a correct diagnosis is the first outcome that matters to patients. European governments are facing difficulties in managing their national health systems, just as the American private payer systems. And the ESR paper points out that short-term cost-cutting solutions, and austerity measures that have been the first reaction, have already reached their limit and are now negatively affecting the quality of healthcare, creating a vicious circle of increased demands on healthcare and a need for greater spending.

‘It’s like low-cost airline companies,’ Derchi compared. ‘They work for a while, then low-cost risks becoming a low-value service.’
After publishing the paper, he has taken to the podium at national radiology congresses to increase awareness of this issue, and to start a dialogue that ESR can bring to all involved stakeholders.
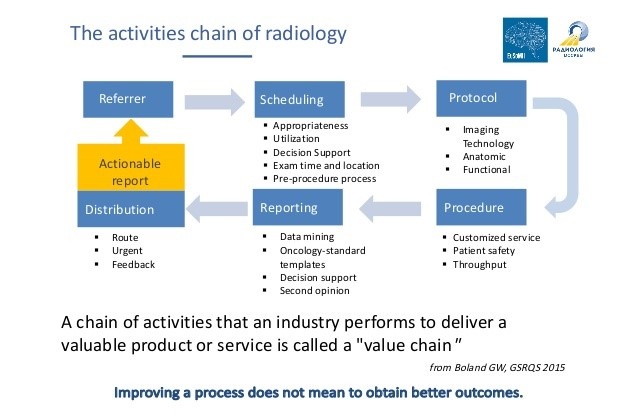
‘As radiologists we have a long tradition of measuring and assessing our chain of work from the request of the referring physician to the report, to measure each step,’ he said. ‘Yet VBH sees these as processes and not as outcomes. What we need to do is define that the endpoint of these processes (the final diagnosis) is an outcome. And we need to ask how we can fit this intermediate outcome into the Value-Based Health Care framework.’
Metrics to measure radiologists’ impact on patient outcomes become a key step to take the discussion to the next level, to demonstrate whether the diagnosis is correct and actionable, that it is relevant and useful to the episode of care.
‘I use the term impact rather than the word value here, because this is the main problem in the ICHOM framework, where value means outcome versus cost,’ said Derchi. ‘They calculate cost and outcomes starting only at the moment when the patient comes to therapy. The impact of the imaging process, or of the other diagnostic methodologies, such as lab tests, biopsies and even the pathology report, needs to be considered not only as a cost but also as something that’s key to the subsequent outcome, affecting what will be done in the treatment process.’
It is our medical knowledge that gives these images significance.
Professor Lorenzo Derchi
The ESR Concept Paper On Value-Based Radiology sets out five key factors in determining appropriate metrics for what it defines as Value-Based Radiology (VBR).
• Appropriateness of requests
• Attention to radiation protection measures
• Characteristics of the reports, whether they are correct, complete, understandable, structured and properly used
• Relationships between patients and radiology personnel
• Continuous professional education, research and innovation.
VBR creates an opportunity to shift from volume-based calculations to a value-based practice of radiology that puts more emphasis on the relation between quality and outcomes. ‘We are doctors in medicine. We are neither photographers, nor operators running machines and pushing buttons. We interpret what is coming from the machines to integrate this information into the clinical picture of the patient to develop the diagnosis. It is our medical knowledge that gives these images significance,’ he emphasised.
‘If you measure only volume, then time is squeezed, the time for the examination is tight, cutting the time for reading and interpreting and for communicating the report. There is no longer time to discuss the findings with the referring physician, to be sure they are understood, and how they may change the opinion on how to treat.’
‘There are two perspectives,’ Derchi concluded. ‘One is economic, and if we are to be measured, we want to be able to show that we have impact on value. The other is an opportunity to discuss this topic, to create a moment for rethinking how we can achieve acknowledgement of our efforts for the quality in our work.’
Profile
Professor Lorenzo Derchi heads Emergency Radiology at San Martino Hospital at University Hospital Genoa in Italy. He also chairs the Value-Based Imaging Working Group of the European Society of Radiology (ESR) and is the ESR’s First Vice-President.
27.10.2017