News • Measuring vital signs
This new technique could render stethoscopes obsolete
No visit to the doctor’s office is complete without a blood-pressure cuff squeezing your arm and a cold stethoscope placed on your chest. But what if your vital signs could be gathered, without contact, as you sit in the waiting room or the comfort of your own home?
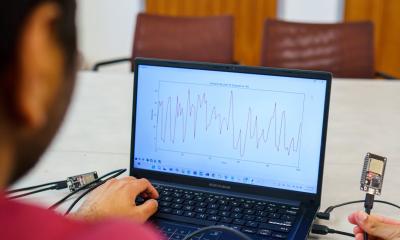
Cornell University engineers have demonstrated a method for gathering blood pressure, heart rate and breath rate using a cheap and covert system of radio-frequency signals and microchip “tags,” similar to the anti-theft tags department stores place on clothing and electronics. The cracker-sized tags measure mechanical motion by emitting radio waves that bounce off the body and internal organs, and are then detected by an electronic reader that gathers the data from a location elsewhere in the room.

The system works like radar, according to Edwin Kan, professor of electrical and computer engineering. But unlike most radar systems that rely solely on radio waves to measure movement, Kan’s system integrates “near-field coherent sensing,” which is better at directing electromagnetic signals into body tissue, allowing the tags to measure internal body movement such as a heart as it beats or blood as it pulses under the skin. The tags are powered by electromagnetic energy supplied by a central reader, and because each tag has a unique identification code it transmits with its signal, Kan said up to 200 people can be monitored simultaneously using just one central reader. “If this is an emergency room, everybody that comes in can wear these tags or can simply put tags in their front pockets, and everybody’s vital signs can be monitored at the same time. I’ll know exactly which person each of the vital signs belongs to,” said Kan.
The signal quality was better than our prediction
Xiaonan Hui
The idea originated after Kan and his graduate student, Xiaonan Hui, visited the Center for Sleep Medicine at Weill Cornell Medicine and NewYork-Presbyterian, where measuring vital signs can interrupt sleep patterns. “We were thinking about the kind of technology we were already using in our lab and thought we could probably get a signal from those vital signs,” said Hui. “But after we figured out the theory and did the experiments, the signal quality was better than our prediction.” The signal is as accurate as an electrocardiogram or a blood-pressure cuff, according to Kan, who said he believes the technology could also be used to measure bowel movement, eye movement and many other internal mechanical motions produced by the body.
Kan and Hui plan to do more extensive testing with Dr. Ana Krieger, medical director of the Center for Sleep Medicine and associate professor of clinical medicine, of medicine in clinical neurology and of clinical genetic medicine at Weill Cornell Medicine. They’re also working with professor Jintu Fan and associate professor Huiju Park from Cornell’s Department of Fiber Science and Apparel Design, who have demonstrated a way to embroider the tags directly onto clothing using fibers coated with nanoparticles. Hui envisions a future in which clothing can monitor health in real time, with little or no effort required by the user. “For every garment in our daily use, there could be a tag on them, and your cellphone will read your vital signs and will tell you some kind of information about your condition that day,” said Hui.
Source: Cornell University
16.12.2017