Article • Health and care sustainability
Short-sighted politicians place NHS in jeopardy
The future of the National Health Service is under threat unless action is taken to address critical issues, according to members of the UK’s House of Lords.
Report: Mark Nicholls
In a hard-hitting report, the House of Lords Select Committee on the Long-Term Sustainability of the NHS criticised the ‘short-sightedness’ of successive governments for failing to plan effectively for the long-term future of the health service and adult social care.
With longer waiting lists for patients and funding shortfalls, a recent survey suggested that 55% of people in the UK also fear the NHS will deteriorate further at a time when there remains uncertainty over the impact the UK’s decision to leave the EU on attracting people from other European countries to work in the NHS.
Tax-funded free at the point of care still the most effective way to deliver care
In its report, the Committee stressed that the UK system of a tax-funded, free-at-the-point-of-use National Health Service remains the most efficient way of delivering healthcare, now and in the future. However, for that principle to remain, members stressed that many aspects of the way the NHS delivers healthcare will have to change. Suggesting that a ‘culture of short-termism’ exists within health and social care provision in the UK, the Lords recommend that a new, independent, Office for Health and Care Sustainability should be established to look at health and care needs for the next 15-20 years. The office should report to Parliament on the impact of changing demographic needs, the workforce and skills mix in the National Health Service and on health and social care funding.
With a merging of health and social care in the UK, the Lords Committee expressed concern that funding between the two has been poorly co-ordinated. The report says that the failure to implement a long-term strategy to secure a skilled, well-trained and committed workforce that the health and care system will need is, the ‘biggest internal threat to the sustainability of the NHS.’ It also advocates a re-shaping of primary and secondary care, and specialised services, and pointed out that service transformation is ‘at the heart of securing the long-term future of the health and care systems.’ Among the 34 recommendations the committee makes are for budgetary responsibility for adult social care at a national level to be transferred to a new Department of Health and Care; NHS England to engage with general practitioners (GPs) to examine alternative models; NHS England and NHS improvement to be merged to create a new body with simplified regulatory functions; the Government to commission an independent review to examine the impact of pay on morale and retention of health and care staff; national and local public health budgets to be ring-fenced for at least the next ten years; a nationwide campaign to highlight the dangers of obesity; the NHS Constitution to be redrafted to emphasise that access to the NHS involves patient responsibilities as well as patient rights.
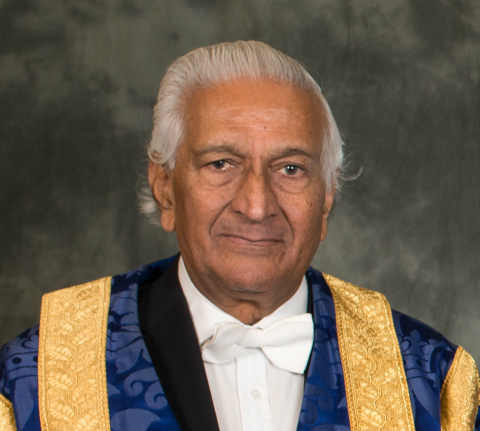
A shocking lack of long-term strategic planning, says Peer of the Realm
‘The Department of Health at both the political and official level is failing to think beyond the next few years,’ confirmed Lord Patel, committee chairman and eminent obstetrician. ‘There is a shocking lack of long-term strategic planning in the NHS. To solve this we need a new body that is independent of government and is able to identify clearly the healthcare needs of a changing and ageing population and the staffing and funding the NHS will require to meet those needs.’
15-20-year plans, but NHS will also need bigger funds especially for low paid

He emphasised the need to look ahead and plan for 15-20 years into the future. ‘We also need to recognise the NHS will need more money. NHS spending will need to rise at least as fast as GDP for 10 years after 2020,’ he added. ‘One area where more spending will be required is on pay for lower paid staff.’ Commenting on the House of Lords Select Committee report, the Royal College of Physicians (RCP) President Jane Dacre welcomed the report’s focus on transformation and the call for a long-term strategy on caring for a changing population. ‘If we are to improve the care for patients we treat, as clinicians, in collaboration with patients, we need to reshape the secondary and specialist care we provide.’ Danny Mortimer, chief executive of NHS Employers, said: ‘It’s imperative the health and social care sector is able to attract and recruit the right staff in order to protect its future, whether that be from the UK or abroad. ‘We also agree that there is a need to give assurances to EU nationals, who make up 6% of the health and care workforce, that they will be able to remain, as well as encouraging them to do so.’
Across the UK, the NHS is currently struggling to cope with patient demand. Funding is rising – an extra £8 billion has been made available by the present conservative government – but this still does not appear enough to cope in a health system that sees a million patients every day and employs 1.7 million personnel (making this the world’s fifth biggest employer). However, despite the issues, the NHS continues to be innovative, leads ground-breaking research and conducts millions of successful – often life-saving – treatments.
Last year saw £140 billion spent on health across the United Kingdom, yet patients at present are waiting longer to see their GP, or for a hospital appointment, for surgery, or to be seen in the Accident & Emergency (A&E) department. A key target stating that 95% of patients arriving at the emergency department should be seen within four hours has not been achieved for two years. However, the number of peoplevisiting A&E have risen by a third in 12 years. Hospitals and health services across the UK are also facing austerity measures and being asked to make savings to balance budgets, often meaning that the criteria for offering routine operations, such a hip replacements or cataract surgery, is being changed with patients having to wait longer, or until their condition has deteriorated further, before surgery is offered.
Health and social care services in the UK are faced with an ageing population; people living longer with chronic conditions; an obesity crisis and rising drug costs. That is combined with difficulties in filling nursing or GP posts, despite the creation of more training positions, and an emphasis towards greater community care but with an infrastructure still centred on a network of district general hospitals.
Plan to draw hospitals and local community teams closer together

NHS England chief executive Simon Stevens has set out a five-year plan to create more integrated care, which involves hospital services working more closely with their local community teams. However, there remains an imbalance in health and social care funding with significantly more money still spent on front-line healthcare than social care.
Profiles:
Professor Jane Dacre was elected President of the Royal College of Physicians (RCP) in April 2014 and is an honorary consultant physician and rheumatologist at the Whittington Hospital in north London, professor of medical education, and director of UCL Medical School in London.
Lord Patel KT – Narendra Babubhai Patel – is a renowned British obstetrician, cross bench peer, and Chancellor of the University of Dundee. He has served as Vice-President of the All-Party Parliamentary Group on Maternity Services since 2002 and in the group on Infertility Services since 2003. He is also Chairman of the Stem Cell Steering Committee since 2003 and a member of the Science and Technology committee.
Danny Mortimer became Chief Executive of NHS Employers in November 2014. His first work in healthcare was as a porter and care assistant before he became a management trainee. He later held a series of director and executive roles before joining NHS Employers, the voice of employers across the English NHS. He also chairs the Cavendish Coalition of social care and health organisations.
14.06.2017