Radiologists are turning into diagnosticians
14:15–15:30
Session 1
Challenges: Radiology in turf battles.
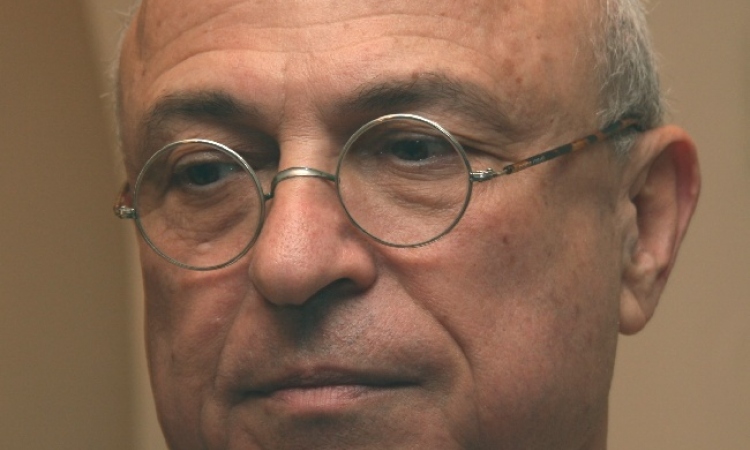
Prof. Jörg Debatin, Medical Director and CEO, University Clinic Hamburg-Eppendorf; Hamburg/DE
Rapid advances in medicine and technology have led to a change in the job description for radiologists. With image acquisition and evaluation increasingly carried out by machines, there is a need to find new fields of activity. However, the required rethink is happening far slower than the pace of development in science and technology, believes radiologist and healthcare management expert Professor Jörg Debatin, the first speaker in the 2011 Hospital Management Symposium.

Licensed as a physician in the European Union, Stuttgart, he became a resident for Diagnostic Radiology at Duke University Medical Centre, Durham, N.C. USA, received an Abdominal Imaging Fellowship at Stanford University Medical Centre, California. Later he became Assistant Professor of Radiology at Zurich University Hospital, Switzerland; Associate Professor of Radiology, Senior Staff Radiologist and head of Magnetic Resonance Imaging at Zurich University Hospital and Professor and Chairman of the Diagnostic and Interventional Radiology Department at University Hospital Essen, Germany.
Since 2003, he has been Professor, Medical Director and CEO at the University Medical Centre in Hamburg-Eppendorf (UKE). Also an expert in and strategist for hospital management, under his leadership the UKE developed several innovative approaches to increase medical quality, scientific performance -- and profitability.
What will ‘medicine as a service’ mean for radiologists?
Prof. Debatin : ‘Basically this is about looking at medicine from the patient’s point of view. The patient is not interested in the label describing a doctor’s specialty on the white coat, but whether a doctor is competent or not. At the same time, we need to understand that the medicine of the future will no longer proceed according to set patterns. This means it will become more individualised. No course of a disease is ever exactly the same. The causes for this lie in the heterogeneity of biology. At the moment we can only guess these differences in cell development by beginning able to identify the genetic profiles of different tumours. All these aspects taken together mean that, in future, medicine will have to be organised in a different way.’
Will payment structures have to be adapted?
‘Yes of course. Whatever creates added value will be paid. Priorities will change quite significantly. The diagnostic process these days will no longer be divided into imaging and non-imaging, but there is a growing need and necessity to link laboratory diagnostics, genetics and imaging with one another. For the radiologist this means that he has to deal more with the content, i.e. with the diseases and their individual characteristics and with possible therapies.
How does this affect daily routine?
‘The former core business of the radiologist, i.e. image diagnosis, loses its relevance. These days, it’s not only image acquisition that’s taken care of by technology but also increasingly the interpretation of images, which is carried out automatically. However, a comprehensive look at all diagnostic data, of which imaging is certainly a significant part, is of great relevance. The challenge will no longer lie in locating a tumour on the image but to integrate the image data with other data, and then to make an individualised treatment recommendation. I think, in future, there will be a differentiation between diagnostics, which ends with an individualised therapy recommendation and planning, and, on the other hand, further therapeutic implementation and care. This will be the case for examinations of all types of organs. It will become important for radiologists to define themselves more as diagnosticians and less as image providers.’
How is the political world following this model?
‘German hospitals are paid for the delivery of a complete service. Admittedly, this is not yet linked to the quality of results, but development is increasingly heading in that direction. Lump-sum contracts with fixed sums are entered into that oblige the service providers to care for patients over a certain period of time. Within this model there is no room for people who do not produce added value. Even today, although an oncologist may read a radiologist’s report on the development of a tumour, he is likely to double check the tumour size himself because he doesn’t trust the radiological data. This current approach is a good example for a scenario where a double effort is made without achieving double the added value.’
So what skills does a radiologist need?
‘The actual intellectual challenge for the future radiologist must be in integrating the volume of available data and assembling it into an overall diagnostic picture. The radiologist is predestined for this. More than any other hospital specialist, the radiologist is used to dealing with different departments. Therefore he is much better trained in interdisciplinary cooperation than doctors specialising in laboratory work, for example. The radiologist communicates with doctors as well as patients. Being able to process large volumes of data quickly, working in an interdisciplinary manner and then explaining results to patients in a comprehensible way - this is where the big opportunity for future radiology lies.’
Why is the self-image of radiologists often so different?
‘Changes are never easy. But radiologists also don’t want a de-intellectualisation of their field. It’s pointless to train someone to become a doctor for six years, and then take five years to specialise as a radiologist if, in the end, they’re just stuck behind two screens. Diagnostic radiologists should not, and will not, volunteer to be pushed into such a corner. It is in the interests of sustainable radiology to achieve a rethink before it is too late.'
11.02.2011