Article • Finances
Operating theatres efficiency impacts on quality care
Given mounting financial pressure, a hospital needs greater efficiency in medical service structures. Staff and materials for operating theatres (OTs) account for about a third of the overall expenditure. Working closely with all other hospital departments, OT efficiency can affect a hospital’s overall efficiency and costs.
Report: Cornelia Wels-Maug
Operating theatre management was established to ensure better deployment of theatre resources by
- Ensuring patient safety during surgery
- Ensuring that all clinical departments have access to the OR-facilities
- Maximising the use of theatre resources
- Minimising waiting times for surgical procedures
- Enhancing satisfaction among patients and staff.
However, to measure the efficiency of a given OT, as well as the quality of its performance clearly defined, measurable indicators are needed to establish a reliable set of benchmarks as opposed to relying on qualitative impressions as to how well or badly the perioperative process has been executed.
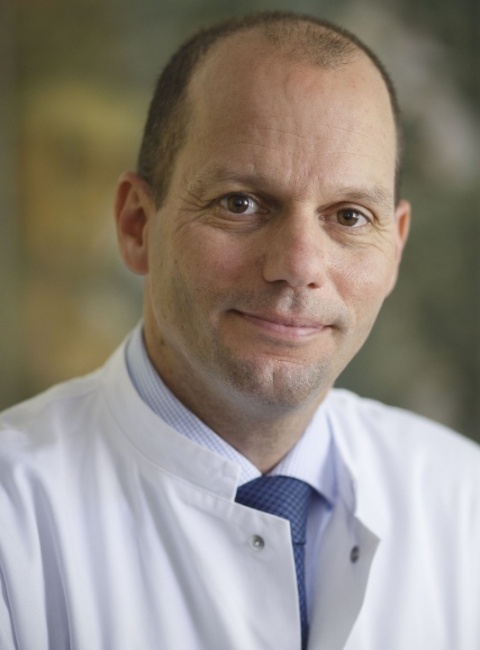
Professor Martin Schuster MD, Head of the Department of Anaesthesiology, Intensive Medicine, Emergency Medicine and Pain Management, at the Fürst-Stirum-Klinik, Bruchsal, Germany, was among a group of physicians and OT managers who set up a benchmarking programme for perioperative process data: ‘It’s really hard to know how many resources are used per patient per surgery,’ he explained. ‘For this, you need to know all the different processes involved in a procedure, from entering the pre-operative unit all the way to leaving the operating theatre. To obtain reliable, reproducible data, a group of hospitals has united to define the different underlying processes and agree on indicators to build up a repository for benchmarking data.’
Beginning in 2009, with 20 hospitals and about 192,000 data sets, there are now (in 2016) 220 participating hospitals, which produce more than 1.5 million data sets per year.
Although the definition of the key indicators for the benchmarking platform are handled by a clinical consortium consisting of the Working Group on Key Figures of the Association of OT Management (VOPM), the German Association of Anaesthesiology and Intensive Medicine (DGAI), the Professional Association of German Anaesthetists (BDA) and the Professional Association of German Surgeons (BDC), all aspects associated with the collection of data are taken care of by Hamburg-based digmed.
This company is responsible for ensuring that the used infrastructure is compliant with current safety and privacy legislation. ‘At the very beginning, we handled the data ourselves at Göttingen university hospital,’ Schuster added, ‘but when this became too contentious, we decided to transfer the job to a neutral intermediary − digmed.’
Hospitals transmit the data electronically to digmed. Those measurements have already been generated as part of a hospital’s routine documentation of each OT case and reside in its hospital information system. However, the data transfer is not in real-time, but typically occurs once a month. In turn, the Hamburg firm performs a centralised plausibility test of the data, e.g. ‘anaesthesia administered prior to incision time’ points to a problem in the data set and the reporting hospital is asked to check its data.
It’s really hard to know how many resources are used per patient per surgery
Prof. Martin Schuster
Designated users of all registered hospitals can access the database via an internet portal to look at their institutions’ data and compare them to the overall benchmark. ‘The data is used to generate reports as well as benchmarks. We also offer the option to compare an institution with its peers. For example, a university hospital can measure its performance with that of other university hospitals’, Schuster points out.
However, the data is not accessible for non-participating institutions. ‘Modifications and the achievement of objectives can be monitored continuously and made generally available by means of an adequate communication structure’, he stresses.
To ensure a high rate of acceptance among hospitals, the benchmarking process is governed by the underlying principles of ‘origin and quality of data’, ‘usefulness and benefit’ and ‘safety and acceptance’. The actual set of key indicators for process efficiency presently comprises 38 measurements, among them ‘Start-time tardiness’, Suture-to-incision time’, ‘Changing time’, ‘Incision-to-suture time’, ‘Degree of OT capacity utilisation’, ‘Number of surgical interventions’, ‘Total incision-to-suture minutes per case’ and ‘Staff costs per surgical intervention/incision-to-suture minute’. Schuster calls attention to the fact that distribution curves are often more meaningful than absolute values and shares some snippets of the insights from the benchmarking exercise.
‘Delays in transporting the patient to the operating theatre are the number one cause for tardiness of surgeries. Additionally, there is often no positive linear relationship between the frequency with which an operation is performed and the time the procedure takes.’
By using the data provided by digmed, participating hospitals have the tools to render their OT processes more efficient, hence, creating additional value for their institutions. However, as useful these key indicators may be, Schuster also warns: ‘They are important tools, but there are pitfalls associated with them because one needs to know exactly how to interpret them, especially around utilisation rates and turnover times.’
As the quality of the benchmark is positively linked to the number of participating hospitals, it will be important, for the future, to win additional institutions and, with it, additional data sets. This will also open the door for applying analytics to the data to uncover hitherto undetected relationships between the process times and the quality of medical care.
22.08.2016