European certification for medical products
The recent scandal around faulty breast implants from France started it, first the talk about the entire medical devices industry, and then progression towards the monitoring and licensing of products.
Report: Brigitte Dinkloh

Although, in the case of the implants, the issue revolved around only one of the estimated 500,000 faulty medical products on the market it was not least the European legislation for the approval of medical devices that attracted attention. In 2011, the Council came to a conclusion and this summer a European Parliament resolution came about the faulty silicone breast implants.
This September, the European Commission (EC) reacted, publishing two Regulations on the revision of the European legislation on medical devices and in-vitro medical products. If these new directives do indeed come into force, this could fundamentally change the certification of medical devices. To date, licensing in Europe, for products in risk class I, for example, has been handled based on the manufacturers’ self-certification: ‘The manufacturers declare the conformity of their products in accordance with the European requirements on medical devices in conjunction with harmonised norms.
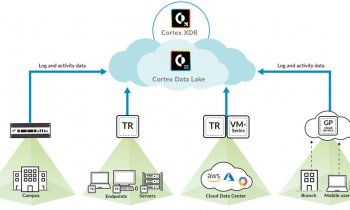
The conformity evaluation procedure is dependent on the risk class of the respective medical device,’ explains Dirk Meier, Senior Consultant for Quality Assurance and Regulatory Affairs at the international consulting company Emergo Group. In the case of products in risk class I it can be sufficient to comply with the basic requirements of the medical devices directive by implementing a certified quality management system for medical devices (ISO EN 13485), without having to consult a Notified Body; for higher risk classes the product file, for instance, must be approved by a Notified Body. Europe has around 80 of these bodies where manufacturers can have their product files checked. Only after they have certified a QMS system as per ISO EN 13485 and confirmed the accuracy of the conformity evaluation, can the manufacturer label the product with the CE mark. According to Dirk Meier this procedure basically works quite well because most manufacturers naturally have a vested interest in introducing safe products to the market.
However, based on recent incidents involving the safety of medical products, it makes sense to increase safety through a revision of the directives. ‘But no system can completely protect us against strong criminal energy,’ he emphasises, ‘even stricter regulations will not reduce the number of “black sheep” down to zero.’
Could the US FDA also be a model for Europe? Unlike Europe, medical device licensing in the USA is not based on the manufacturers’ responsibility but implemented through the central Food and Drugs Administration (FDA). The FDA regulations are different from those effective in Europe, particularly in the case of product changes, where a stricter testing scheme is applied.
Nonetheless, centralisation does not necessarily make the licensing procedure any easier: ‘The American licensing system is easier to manage for larger companies than for smaller ones. If we were to envisage a similar solution for Europe, the need for consulting and advice would increase significantly and, in the case of medium-sized companies and small startups, the barriers for licensing would be raised.’ However, 80% of medical devices and technology companies and 95% of in-vitro diagnostics manufacturers in Europe happen to be medium-sized, small or micro companies. In 2009, they achieved a turnover of €85 billion for medical devices and €10 billion for in-vitro diagnostics equipment.
Dirk Meier therefore pleads for a different solution: ‘It certainly makes sense to increase product safety through a re-organisation of the Notified Bodies whilst simultaneously extending their competencies. For instance, increased product safety could be achieved through longer audit periods at the manufacturers’ premises and a periodical change of auditors. In the same way, the planned changes involving the introduction of unannounced audits at the manufacturers’ premises are a further contribution towards patient safety.’ The European Commission estimates that the establishment of a central registration body could save administrative costs of around €157 million. A similar effect is expected from the establishment of a central monitoring portal, instead of the current national portals, such as the BfArM (Federal Institute for Drugs and Medical Devices) in Germany.
The consultant is also in favour of a unified listing of all licensed products: ‘It’s much easier in the US to obtain information on the licensing of products and on incidents.’ The suggested regulations also take into consideration more strongly than before the convergence of regulations with the major trading partners. For 20 years the EU, in the context of the Global Harmonisation Task Force (GHTF), has been working to improve the safety and quality of medical devices, to ease technical progress and break down international trade barriers.
Medical insurers demand improvements to protect patients
Europe’s statutory medical insurers are less satisfied with the EU draft for the revised medical devices directive. In a joint position paper (pub: 22 October) they demanded the introduction of an accreditation requirement for high-risk medical products on a European level and an improvement of the rights of injured patients. They deem the current system, which is based on certification by notified bodies, as insufficient for effective patient protection.
The insurers argue that, over and over again, medical products that cannot be marketed in the USA, but which initially have to be licensed in Europe, end up having to be taken off the market for safety reasons. ‘The revision of the European directive on medical devices is a very fitting opportunity to completely revise the current certification and monitoring system for high risk medical products and to introduce a genuine marketing authorisation procedure,’ the medical insurers write in their joint position paper.
In place of the current CE certification procedure through private, notified bodies, more than 50 umbrella organisations of the medical, retirement and accident insurers from 15 EU Member States (European Social Insurance Platform – ESIP; Association Internationale de la Mutualité – AIM), the publishers of the drug bulletins (ISDB) and the Medicines in Europe Forum (MiEF) are calling for a central licensing procedure for high risk products on a European level that is to govern the safety and effectiveness as well as the positive risk-benefit ratio based on the results of high quality, clinical studies.
Based on the current regulatory guidelines of EU law it remains unclear exactly when a clinical evaluation of a medical product to confirm its compliance with the basic requirements according to Appendix I of guideline 93/42/EWG is actually required, the medical insurers argue. Previously when clinical evaluations with medical products were actually carried out, testing was mostly limited to only a small number of patients without control groups and, particularly in the case of implants, this was also limited to short observation periods. Additionally, medical device manufacturers too often took the opportunity to submit existing scientific literature, rather than actually having their medical products tested by the notified bodies.
To this extent, in the eyes of the medical insurers the commission’s proposal hardly contributes towards an improvement in the current shortcomings regarding clarity. They also argue that the licence for high-risk medical products initially should be limited to a period of five years. After that, manufacturers should again have to prove the safety and effectiveness of their products.
PROFILE
Dirk Meier, BSc (Mech. Eng.) MPhil, worked as a development engineer & medical device regulatory specialist at Terraklin AG – Gambro GmbH and regulatory affairs manager & QA specialist at Hoffrichter GmbH before becoming Senior Consultant for Quality Assurance and Regulatory Affairs at Emergo Group Inc. His areas of expertise range from respiration therapy and artificial extracorporeal liver support to heart support systems. His disciplines: CE Marking - Technical Files and Design Dossiers, FDA Quality System Regulations – 21 CFR Part 820, US FDA 510(k) submissions, EN ISO 14971 Risk Management, Clinical Evaluation, MEDDEV. He is also a peer reviewer for Artificial Organs, in Boston, USA.
16.11.2012