Article • Fragile state
Many units themselves need emergency care
Germany’s hospital emergency departments run up a loss of more than one billion euros every year. According to Dr Thomas Fleischmann, specialist in the reorganisation of emergency departments, care for emergency patients rakes up a loss of about one billion euros every year.
Report: Ralf Mateblowski
Comparing apples and oranges
‘The loss generated in emergency departments is primarily caused by a significant increase in out-patients – who today account for two thirds of all patients presenting to the emergency room. The major problem is the reimbursement system via the German physicians’ associations, the Kassenärztliche Vereinigung. To be more precise: physicians in the emergency room are reimbursed exactly like office-based physicians. However, the emergency room is open 24/7, 365 days a year, whilst a doctor’s office is open 30 hours a week.’
A second difference, Fleischmann points out, ‘Are the provision costs of an emergency department, be it for physicians or nurses, for CT, cardiac cath lab or intensive care. The moment you subtract these provision costs from the total costs and add comparable costs for 24/7 care to the profit and loss account of a doctor’s office the difference between hospital emergency room and doctor’s office is not that big any more. Currently, costs in very different infrastructures are reimbursed identically – but whilst this reimbursement might be sufficient for a doctor’s office it will never even come close to covering the additional staff and operating costs a hospital’s emergency room incurs with its around-the-clock service.’
Internal considerations
‘When we look at internal factors, our emergency departments don’t look too bad. Overall, we provide good healthcare. However, there is room for improvement. Unlike other industrialised countries, in Germany it’s mostly the junior physicians rather than specialists who staff the emergency room.’
Specialists are in short supply
‘Germany is one of the few countries – not just in Europe, but also among high-income countries worldwide – that does not provide regulated training for emergency room staff. The result is that inexperienced junior physicians, trying not to make mistakes in the emergency room, tend to do too many exams of patients with low-degree conditions and to admit too many people as in-patients. This issue can only be solved with adequate and defined training in clinical emergency medicine.’
Going forward
‘Most importantly, emergency care must be financed; we must not allow it to starve to death. Secondly, the quality of care has to be raised to specialist physician level for each patient to receive exactly the type and level of care he or she needs – not more, not less.
‘Let’s look at the triage categories: red, orange and yellow – these are patients with medium to severe conditions. Green and blue are patients with minor problems and injuries. Patients with medium to severe conditions account for about 60 percent of cases; the remaining 40 percent are greens and blues. It’s the latter category that is rapidly increasing. In my opinion, care for patients in the triage categories red and orange is very good, but we do offer too much medicine to the others.’
Light at the end of the tunnel
In Germany we cannot – and must not – wait for an international solution; we must find our own direction
Thomas Fleischmann MD
‘The problem of under-financed emergency rooms is not a German problem, but a problem that’s present in many high-income countries, such as the USA. In Germany we cannot – and must not – wait for an international solution; we must find our own direction. To be fair, we are witnessing a historic change: The coalition contract between the German government two parties mentions emergency departments – for the first time ever! Emergency care is recognised as one of the four pillars in the hospital structure law. That is new. While modifications to the hospital structure law are not sufficient, they are a clear step in the right direction. They show that German politicians have recognised the problem.’
Conclusion
‘Beyond the fundamental and politically necessary changes, there are no simple solutions for the individual emergency room. Optimisation of emergency care will not result from one single measure but rather from the result of the package of measures to increase efficiency, lower costs and improve financing. Germany has to overcome two major challenges: The extreme shortage of emergency professionals – both in the medical and in the nursing sector – must be addressed. And secondly, no matter how we look at it, we must not allow emergency care to be atrophied for business reasons.’
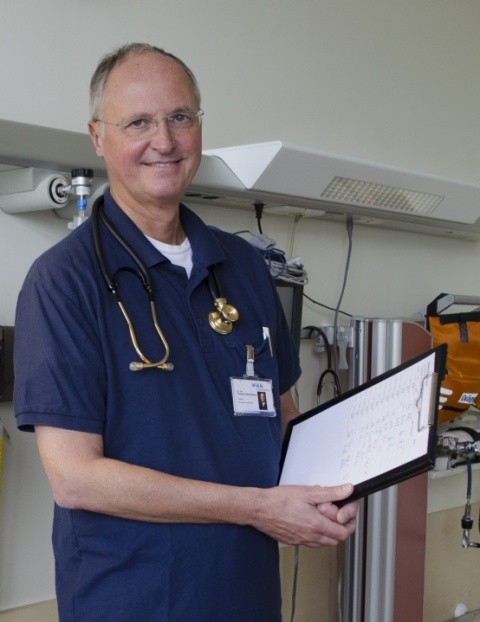
Profile:
Thomas Fleischmann, MD was among the first German physicians to pass the European Board Examination in Emergency Medicine (EBEEM) and, in 2014, he completed his Master of Health Business Administration (MHBA) course – top of the year’s class. Having formerly successfully reorganised emergency departments in Salzgitter, Frankfurt-Höchst, Sanderbusch and Hirslanden (Zurich, Switzerland), he was appointed Medical Director of the Emergency Medicine Department of Westküstenklinikum Heide, this summer. A specialist physician for general medicine, emergency medicine and clinical emergency medicine, and Fellow of the Royal College of Emergency Medicine (FRCEM, UK) and of the European Society for Emergency Medicine (FESEM), he has received many awards for his dedicated work. He has also edited several textbooks on emergency medicine and co-authored the European curriculum for this specialty.
20.01.2017