’French twist’ in e-Health
Can a low-cost patient file provide the route to creating the complete medical record?
It seems medical records are too serious to be left to patients. Across hundreds of European e-health projects, the heavy spending in health information technology goes to building an electronic health record (EHR) that can be shared among health professionals.
Invariably the projects start with a complex infrastructure to capture hospital and physician records at a cost of some hundred of million of euros.
Meanwhile the patient health record (PHR), the part of the medical record that patients are welcome to see, is filled with summary reports and educational materials – lightweight stuff in the scheme of things. Yet, facing the complexity and prohibitive costs of building an EHR, France turned to the PHR, creating a large-scale project for the dossier medical personnel (DMP).
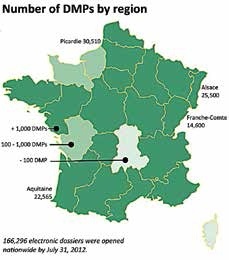
It is an invention born of necessity. First, a law passed in 2002 clearly states that each citizen shall have a DMP. Secondly, France has under-invested in hospital information systems for many years, crippling its capability to generate and share records. With a government in crisis, there is little hope for the funding to catch up. The first €100 million spent to create the DMP ended in disaster with a death certificate for the programme in 2007 signed by three ministers. Yet, five years later and another €100 million further on, the DMP is now up and running with 166,296 dossiers, a number that is expected to double by the end of the year, but still far short of expectations for a population of 65 million. ‘I would love it if things would go faster,’ said Jean-Yves Robin, the head of the agency responsible for bringing the programme back to life, ASIP-Santé (Agence des Systèmes d’Information Partagés de Santé). However, Robin, who sees the online file as a carry-all, a tool for health professionals to coordinate care, cautions it will take another five years before the DMP is systematically built into clinical practice across France.
Development by individual hospital
Since December 2010, technically any French citizen can open a DMP; but instead of launching a public campaign, which would have created a nightmare, according to Robin, the DMP is being deployed hospital-byhospital using the newly created network of autonomous regional health authorities. In a first phase that ended in July, four regions completed the integration of the DMP into their hospital information systems at a cost of €7.5 million for ASIP-Santé. In September, ten further regions will join the deployment programme at a cost of €15 million for education and training, as well as creating an interface for hospital systems and providing updated software for physician offices.
‘It is not hard to see that the total of this funding is relatively low compared to countries that are spending hundreds of millions to deploy their systems,’ said Robin. The comparison with the United Kingdom’s 10-year and £12 billion Connecting for Health programme is inevitable. ‘They have had their difficulties, yet they have also made great progress,’ he said, adding that the advanced infrastructure for hospitals ‘is something we would dearly love to have in France.’ The country, he added, ‘suffers from its under investment in hospital information systems, to the point that there is an insufficient capability for hospitals in creating medical records for the DMP.’ He believes the famous NHS ‘spine’ works very well, ‘but the decision to build a dedicated network in the UK was the result of historic circumstances. Today I don’t see this as being something we need to do. The health services in France can be perfectly well built on the Internet.’
Over the past year the infrastructure for the DMP has proven to be reliable, even if it has not been overly taxed for robustness. ‘We are out of the pilot stage and in full deployment, ‘ said Robin, adding, ‘I want to emphasise that we are just at the beginning. Many of the files created by patients are only two months old.’ The region-by-region roll-out strategy has demonstrated that it costs an average of €100,000 for a hospital to come online with the DMP, a relatively small part of the annual budget for health IT. Spread across the 2,900 hospitals and clinics in France, Robin said a five-year total of €290 million to integrate the DMP proves to be very cost-effective.
PROFILE
Jean-Yves Robin MD, the Director of l’ASIP Santé (Agence nationale des systèmes d’information partagés de santé), began his medical career by fulfilling numerous missions in developing countries. Fascinated by the potential for new technologies to enhance medical communication, in 1998 he founded Uni-Médecine, specialised in health information systems. Pioneering work in establishing pharmacy records and significantly a shared file for cancer patients for the National Cancer Institute won a recognition for Uni- Médecine as an innovative enterprise. The company was acquired by Atos Origin in 2007. The following year, Robin accepted the formidable task of reviving the French programme for a national health rec-cord and, against all odds, successfully launched the DMP two years later.
12.11.2012





