Percutaneous therapy for pelvic fractures
By Patrick D Eude, Centre Hospitalier H. Mondor, Aurillac, France
Fractures and disruptions of the pelvic ring are most often unstable, and can therefore jeopardise patients' standing and walking functions.
They are frequently caused by high intensity mechanical trauma. However, some lesions cannot be considered unstable because they do not sustain any load: lower anterior and posterior fractures of the acetabulum, even if associated fragmental fractures of the pelvic bone, are no threat and only need bed rest.
Displaced and comminuted fractures most often require open reduction and internal fixation (ORIF). The only emergency situation is hip dislocation that demands quick reduction. However, these are dangerous and difficult procedures.
Because of these dangers, the most usual treatment of non or slightly displaced fractures is continuous longitudinal traction. During a 30-45 day period, the patient stays in bed sometimes with a traction device set on a transosseous Kirschner wire. Prolonged bed rest, however, has its own complications, sometimes lethal in elderly patients. Conservative treatment is often unsatisfactory, and ORIF is an obviously more aggressive method.
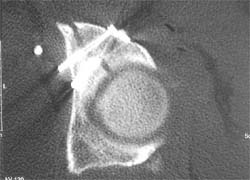
The development of CT-guided surgery attempts to avoid most of these complications. This technique aims at a quick fixation of pelvic fractures, allowing early standing. Precise guidance and easy control of the different phases of the operation lessen the operative complications and allow a more accurate positioning of the fixation device.
Procedure - Our experience is based on a series of 86 patients, 63% male and 37% female, between 14 and 94 years old. Almost 50% were traffic accidents and 40% were falls (most frequently sport and work). We noticed 10% of these patients attempted suicide; these are obviously most fragile patients whose comfort must be considered as an element of therapy.
After initial X-ray diagnosis, helical-CT evaluation of the whole pelvis was quickly implemented, with multiplanar and sometimes 3D reconstructions. Non or slightly displaced but unstable fractures were proposed for surgery and, in most cases, a traction device was set. Feasibility of percutaneous fixation and optimal approach(es) were discussed with surgeons and interventional radiologists. According to the patient’s status, the operation took place between three days and three weeks after the accident.
Spinal anaesthesia was sufficient in over 90% of cases. After carefully and precisely positioning a guide-pin just beyond the fracture line through a small skin opening, a cannulated screw was driven on the pin and tightened. One to four screws were inserted, according to the type of injury. CT slices were used to control the pin, the drill and the screw position. Each cutaneous opening required one or two stitches. Anaesthesia allowed us to remove the traction device at the end of the operation. In only one case of a highly comminuted fracture did this device have to be kept for 18 days. Further consultations are planned after 15, 30, 45, 60 and 90 days. Such an operation takes from 20 to 60 minutes, and the total occupancy of the CT room is two to three hours.
Results - Blood loss was less than 25 cc in all cases. No vessel or nerve injury was noticed; no infection was reported, and no screw had to be removed. Painkillers were required only during 36 to 48 hours. No antibiotics were necessary unless for other reason (open fracture, thoracic or abdominal injury).
In 90% of the cases the patient could sit on the day after (day one), in three cases on day two, in four on day three or four. Other injuries prevented one patient from sitting before day 18. They could resume walking with crutches on the same day and were discharged from the surgical department as soon as they could ambulate safely. Walking on both legs was allowed after 30 (simple fractures) to 45 (complex fractures) days.
After a 100 to 240 day follow up, 87.5% of patients were satisfied (14 cases), since they had recovered their previous everyday activities, and even most sports and work capacities, with no or only occasional pain. Dissatisfaction was due to residual pain.
Conclusion - In the light of this experience, we can conclude that:
• Close cooperation between surgeons and radiologists is mandatory
• Only usual instruments are required to insert the screws
• Prudent positioning of pins and screws, guided by CT-slices, should avoid complications
• The occurrence of an infection is extremely low (no case in most published series), therefore antibiotic therapy is not systematically required
• Quick pain relief and usually short stay in bed (2 days instead of 30 to 45) notably increases patient’s comfort and shortens the period for recovery since rehabilitation may be initiated at once
• The considerable reduction of hospital stay (seldom longer than 6 days) generates important savings
• CT guided percutaneous screw fixation of pelvis fractures therefore appear as a quick, safe method if carried out by well-trained radio-surgical teams.
Contact: eude_p@hotmail.com
01.05.2006


