Radiology & nuclear medicine - Sharing an awkward waltz in Vienna
CT-PET is the child of a forced marriage between nuclear medicine and radiology. A shared session at ECR 2011 in Vienna did little to assure there is a growing consensus between the two partners.
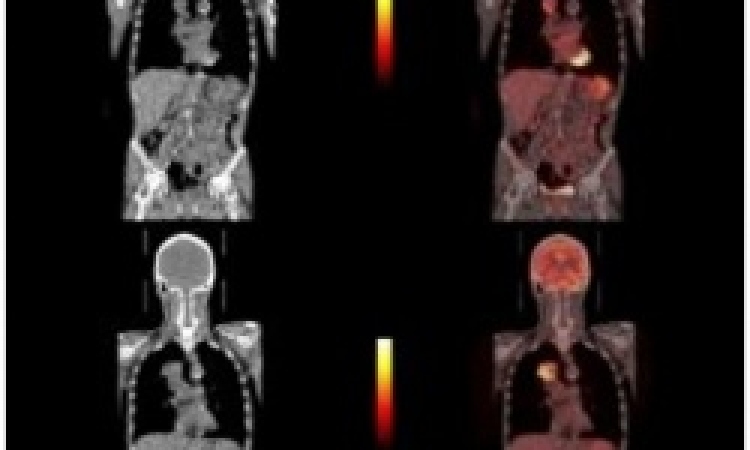
The fusion of positron emission tomography (PET) with computed tomography (CT) has brought tremendous benefits to patients.
Last year, over 3.2 million CT-PET scans were performed worldwide, by combining functional images of blood perfusion in tumours and other diseased tissue from nuclear medicine with anatomical images from radiologists.
Yet, despite years of sharing this advanced technology and often working side-by-side, there remains a sharp division between these two specialised fields of medical imaging. ‘Those people in nuclear medicine have really ugly images, just ink spots,’ complained one radiologist.
Meanwhile experts in nuclear medicine complain that CT exams offer little more than additional information of anatomical structures to more critical data provided by nuclear agents.
At the European Congress of Radiology (ECR), for the second year in a row, the European Society of Radiology (ESR) and the European Association of Nuclear Medicine (EANM) organised a joint session to bridge the gap between their two specialties. This was a success for reviewing the achievements in both areas, but only a modest step toward reconciling the two fields, in that no collaborative project was presented.
Instead, the societies took turns putting forward their champions in an alternating and slightly artificial fashion for studies in tumour response.
Martin O’Connell MD, from Mater Misericordiae University Hospital in Dublin, Ireland, was put forward as the expert radiologist. In tracing the effectiveness of therapies for tumour response, ‘nuclear medicine leads the way here, no question,’ he said.
After reporting the effectiveness of CT-PET for determining, after just two treatment cycles, or three weeks, whether patients respond to the therapy, Dr O’Connell devoted the remainder of his presentation to a review of alternatives.
CT scans unaided by contrast agents is well established as the gold standard for Response Evaluation Criteria In Solid Tumours (RECIST), he reminded colleagues.
Tracers in the blood showing accumulations are not always reliable indicators of the disease state, he said, and there is a danger for some patients of overdoses from radioactive probes used in perfusion studies.
Diffusion weighted MRI studies, especially for whole body scans, can often outperform PET studies, he suggested, before concluding with a pointed comment suggesting that multi-disciplinary meetings are essential, urging his nuclear medicine colleagues with: ‘You really need to attend the meeting.’
Autoro Chiti MD, with the Nuclear Medicine Unit at Humanitas Clinical Institute in Milan, gave a nod to his radiology colleagues by acknowledging that oncologists have come to trust CT exams for their reliable quantification of tumours. He then reminded the audience that RECIST standards were established in a paper from 1976, where hand measurements were used. ‘Today, of course, we have sophisticated tools for measuring, but this is the heritage,’ he said, adding that there remain serious limitations for RECIST in relying upon morphological measures provided by CT. ‘Tumours take time to shrink, and an early measure showing no reduction risk leads to the wrong conclusion as to whether a patient is a responder or a non-responder to treatment,’ he said.
CT-PET is really about the measure of the activity inside the tumour, the glucose uptake of the target lesion, which is shown by the injected nuclear agent.
CT is useful to show changes in tumour size at the end of treatment, or after six months, he said, where it is chemo-sensitivity that enables the early prediction of effectiveness of treatment. ‘This gives a completely different measure with the expression of activity,’ he pointed out.
As an example, Dr Chiti showed a tumour assessment after a two-cycle of chemotherapy, where the lack of change in the internal activity encouraged a change in treatment. Two further treatment cycles with the new formulation showed significant reduction of tumour activity, which, he said, ‘is a predictor of the effectiveness of the changed treatment.’ And yet, he added, ‘the size of this targeted lesion as shown by CT did not change.
‘Imaging,’ he concluded, ‘provides important additional information.’
The presentations by two champions of these cooperative, although clearly competitive specialties, established that the fusion of metabolic and morphological data is helping to improve diagnostic accuracy for cancer patients.
However, the joint session of the two professional societies left more questions than answers about the consensus recently established for a Multimodality Imaging Training Curriculum, which ESR President Maximilian Reiser announced would be published soon in the online journal, Insights into Imaging.
John Brosky reports
20.04.2011