Medical research
Pharmacogenetics - Researchers focus on customised medication for patient groups
In the first month of 2011, the Centre for Pharmacogenetics and Pharmacogenomics at the Paracelsus Private Medical University in Salzburg, Austria, officially opened its doors. Why have pharmacogenetics and pharmacogenomics so increasingly important in medical research? We asked the head of the new research centre, Professor Markus Paulmichl.

‘There isn’t one drug that helps all patients,’ said Professor Paulmichl. ‘One group of patients may respond to a drug as desired. However, the next group might feel no effect whatsoever, and the third group may end up with complications. This obviously makes one wonder whether this may have something to do with the individual genetic make-up. Therefore we examine whether the said patient groups have mutations in those genes involved in the absorption, distribution and metabolisation of drugs in the body.
‘For example, the liver enzyme CYP2D6 required for the metabolism of xenobiotics metabolises around 20% of drugs used in Europe. In six to eight percent of Caucasian Europeans this enzyme works insufficiently and they can expect side effects. Around 4% of Europeans have an excessive function so that the drugs are metabolised too fast and don’t amount to a therapeutic concentration. These are significant figures.’
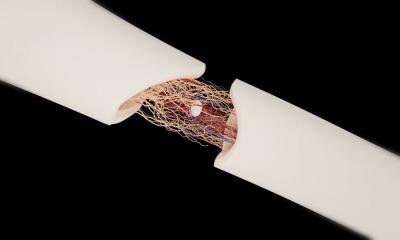
Asked about the research projects currently being undertaken at the centre, he said: ‘At the beginning of pharmacogenetic research the emphasis was on metabolising enzymes. However, we focus on those structures responsible for the absorption and distribution of drugs. This is a new field to which great importance should be attached. One of our central areas of research is the blood/brain barrier. There are pathological changes in the brain that we’d like to be able to control pharmacologically. However, the blood/brain barrier ensures that many substances in the blood do not get into the brain. A second area of research is the bronchial epithelium, because some drugs are applied to the lung via inhalers, as in asthma treatment, and the target cells are not directly at the surface. The genetic make-up obviously also has an impact here.’
So, is pharmacogenetics a step in the direction of personalised medicine?
The development is definitely heading towards the direction of a strong segmentation of the patient pool.
Wouldn’t such segmentation lead to higher costs?
Overall, we could put a black zero under the line for healthcare. Clinical studies could be carried out on a smaller scale because they are no longer expected to cover the effects in the entire population on a broad scale. This could result in significant savings in the development costs for new drugs. A lot of money could also be saved through the reduction of side effects. If you project the data from the USA, then we spend around €100 million on the treatment of side effects from medication -- in the Salzburg region alone. This is a considerable sum. But the money saved in the process will have to be invested in diagnosis. However, the discussion shouldn’t always be reduced to talking about costs. The advantage for patients is evident: They are given the drugs with the least side effects.
What possible obstacles do you foresee?
It will make things more complex for clinicians. One problem is likely to be the training and advanced training of doctors who have not had to become involved in pharmacogenetics, so far. They will have to be convinced of the advantages that this new approach results in for the patients.
20.04.2011