Novel cancer treatment options
During a gathering of clinicians, scientists and economists at this year's Medical Technology Congress (Treffpunkt für Medizintechnik) held in Berlin's Charité Hospital, all 17 lectures focused on cancer treatments. Bettina Döbereiner reports

Organised by IHK Berlin, the city’s chamber of commerce and industry, and the specialist medical technology centre TSB Medici, this year’s Medical Technology Congress attracted around 200 doctors, researchers and firms. Siemens Healthcare, for example, presented new syngo imaging software to assess tumours automatically, e.g. lung, liver and lymph nodes, as well as to measure their volume and percentage change in volume.
Two relatively rare tumours – Prof Roland Hetzer (German Heart Institute Berlin) presented his ablation procedure for cardiac tumours and metastases (262 heart tumour operations have been performed at the institute since its 1986 opening), and Prof Michael Foerster (Benjamin Franklin Berlin eye-clinic) demonstrated the use of proton therapy to treat ocular tumours.
Cephalic tumours – Prof Oliver Kaschke (Gertrauden Hospital Berlin) introduced laser- and micro-surgery for cephalic tumours. Potential therapy planning using digital volume tomography for benign and malignant head/neck tumours were presented by Prof Erwin Keeve (Charité University Hospital) and Prof Ulrich Kellner (neurosurgery clinic) reported on the surgical treatment of neurocranium tumours.
Open MRI – Since 2007 the radiology institute at Charité has co-ordinated an interdisciplinary project to develop surgical instruments for use in procedures using Philips Panorama 1.0-Tesla open high-field MRI – particularly for minimally invasive surgery, and Dr Florian Streitparth discussed the possibilities of open high-field MRI-navigated thermo-ablation and Dr Frank Fischbach (Magdeburg University Hospital) reported on an open high-field MRI fluoroscopic-based liver intervention.
Curative and palliative photodynamic therapies – Prof Hans-Peter Berlien (Laser Dept, Elisabeth Hospital Berlin,) discussed laser technology used as a remedial therapy for dysplasias, pre-cancerous lesions and superficial tumours. For palliative care he cited the treatment of metastases, tumour mass reduction and recanalisation. In general, he said, photodynamic therapies are ideal in combination with surgery or chemo/radiotherapy.
Tomotherapy – Dr Hendrik Herm (Radiation Dept. Helios Hospital Berlin Buch) described the use of tomotherapy to deliver radiation slice-by-slice to different tumour areas, enabling precise irradiation of very large or tiny, inaccessible tumours, whilst sparing surrounding organs. 494 patients have received this treatment since tomotherapy was implemented at Helios in January 2008.
Non-viral gene-therapy with jet injection – Associate Professor Wolfgang Walther reported results from the first clinical trial to evaluate the feasibility of jet injection for gene therapy. Led by Prof Peter M Schlag, the project, a co-operation between Berlin-Buch, Charité – Universitätsmedizin Berlin, the Max Delbrück Centre for Molecular Medicine (MDC) and 4PlasmidFactory GmbH & Co. KG, Bielefeld, aims to test new technology that uses high pressure to transfer genetic material directly into a tumour. Generally, viral vectors are used for these transfers, but clinical studies have shown potential side effects using direct viral technologies. Non-viral vectors may be less efficient at introducing and maintaining foreign gene expression, but they are non-pathogenic and non-immunogenic, Prof Walther said, predicting that ‘naked’ gene transfer will increase in practice. Tools for this include electroporation, gene gun, needle injection, ultrasound and jet injection.
During the clinical phase of the trial, involving 13 patients with malignant melanoma and four with skin metastases of breast carcinoma, only a reporter gene was used. Three days after injection, lesions were removed; analysis showed that jet injection had safely and directly delivered genes into the tumour tissue. On the whole, the application was well tolerated by all 17 patients, with no adverse events. ‘Whereas viral gene transfer may still be limited due to safety concerns,’ explained Dr Walther, ‘the application of naked gene constructs is considered safe.’ Additionally, jet injection can be used for a broad spectrum of clinical applications due to moderate cost and easy preparation. The researchers now want to trigger therapeutically relevant genes in tumour tissue using jet injection-based non-viral gene transfer. Dr Walther pointed out that although small tumours are sufficiently infiltrated by jet-injection, it needs optimisation to reach bigger tumours sufficiently.
Thermotherapy & nanoparticles – Dr André Roggan (Celon AG medical instruments) introduced the basics of thermotherapy and three lecturers presented different forms of thermo-based tumour ablation. Worldwide, about 75,000 liver carcinoma ablations are conducted annually (hepatocellular carcinoma, colorectal metastases, metastases of mamma-carcinoma). New clinical studies are underway to treat bone, lung and kidney cancers.
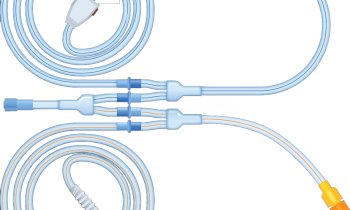
During thermotherapy, heat, from 50ºC up, delivered into tumour tissue via special applicators, destroys the tissue. One minute at 60ºC brings immediate and irreversible tissue damage. The main problem is local relapses, said Dr Roggan. In a 2005 study the average local relapse rate in all patients treated with thermo-based tumour ablation was c. 12%. For tumours over 5cm the probability of local relapses can rise to over 50%. Up to 90% of thermo-ablation technology utilises radio frequency (RF). Celon AG has developed and is testing bi- and multi-polar RF ablation, which introduces a current solely to a cancer site.
Laser and microwaves are also used to deliver heat into a tumour. Instead of special applicators, energy transfer can be activated by transcutaneous ultrasound emission or with external magnetic activation of locally installed nanoparticles.
Dr Jürgen Bunke (Philips Healthcare) discussed a new development in MRI-guided high intensity focused ultrasound (HIFU) to treat uterine myoma. This volumetric, high-intensity focused ultrasound method offers more efficient energy exposure, cuts treatment time and the ablation will be more homogeneous. Uterine myoma therapy is a first step towards treating malignant tumours with the same technology, he added.
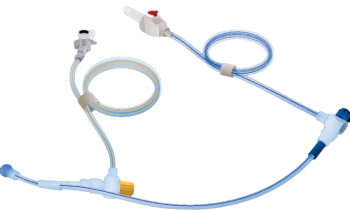
Dr Martin Hossfeld (Magforce Nanotechnologies AG) described novel therapy to damage tumour cells directly with temperatures above 42ºC. Currently in phase 2 trials at two neurosurgical clinics, and involving 72 patients with glioblastoma relapse and prostate cancer, the therapy combines nanoparticles with radiation therapy (30Gy). Using a biopsic needle, magnetic movable nanoparticles (size 10-15 nanometres) are introduced into a tumour – 0,3 to 0,1 ml nanoparticle containing liquid per ml of tumour tissue. Each nanoparticle core of magnetite is coated with aminosilanes, which stabilize them against agglomeration and sedimentation and also ensures they are correctly positioned within a tumour.
Software enables therapy planning and full temperature control applied in the tumour (during the initial treatment a thermal catheter is inserted to align and control the temperature computed by the software). Precise tumour determination is essential before MRI or CT. The patient is placed with the targeted tumour area in the magnetic field and the power can be manually raised until the decided temperature inside the tumour is attained. So far, the maximum temperature deviation is 0.1ºC. The magnetic field temporally stimulates the nanoparticles and, after absorbing that energy, the nanoparticles release it into the tumour as controlled heat.
Presently tumours up to 7 cm diameter are being treated in six one-hour magnetic field sessions, two per week. No anaesthesia or immobilization is necessary. Patients with metallic implants are excluded.
Dr Hossfeld said the advantages of nanoparticle based tumour therapy include a focused local calefaction of almost all solid tumours; the possibility to plan in the range of mm; only a single insertion of nanoparticles; a less adverse reaction and no attendant resistance mechanism. One disadvantage remains: Due to the remaining metal containing particles and subsequently occurring artefacts, MRI diagnoses are limited. This, he said, will be solved when new diacritic systems are established.
Questioned on nanoparticle migration, Dr Hossfeld said that, in animal studies, the majority of nanoparticles were absorbed by macrophages; they attack the cancer cells and remain there. In one patient, in remission from the phase 1 study, 80% of particles remained in situ, he said. The rest would biodegrade.
01.09.2009