The 90th German Radiology Congress
Focus: The role of radiology in oncology
"Radiologists often see cancer patients over a period of years and continuously deliver important information for the treatment process," says Claus D. Claussen MD, Professor of Radiology and Director of the Clinic for Diagnostic and Interventional Radiology at the University Hospital in Tübingen and President of the 90th German Radiology Congress. For the first time in the history of this congress, which is rich in traditions, the programme has been organised jointly with the German Cancer Society. Here, Professor Claussen outlines the importance of radiology in oncology - and what he defines as a change of paradigm in cancer care.

“Cancer has been and will remain a big challenge for medicine. With increasing life expectancy, as well as critical changes in social, environmental and ecological living conditions, the occurrence of cancerous diseases is increasing. Next to the medical problem is the economic problem. On the one hand, innovative treatment concepts must be made available to large sections of the population; on the other, the rising costs for this medical treatment must be met. From a medical as well as an economic perspective, it is essential to achieve interdisciplinary networking of specialist competencies.
Tumour boards
Only the close and trusting co-operation of the oncologist with all surgical and conservative medical disciplines, with radio-oncologists, radiologists and specialists in nuclear medicine, allows an optimum treatment concept, ranging from the initial diagnosis to therapy planning and therapy control. Tumour boards, i.e. regular conferences for representatives of different medical disciplines are outstanding instruments to help combine and align individual treatment plans with the guidelines of the relevant specialist medical associations and to determine the right therapy for the patient.
Individualised medicine – individualised imaging
Cancerous diseases are complex. Consequently, there is a necessity for an individual approach for each individual patient. Imaging plays an essential part in this ‘individualised medicine’ because the radiologist often sees oncological patients over a period of several years and continuously delivers important information about the individual spread pattern of the disease and changes seen during treatment.
Disease-focused, not organ-focused
Malignant diseases are – apart from a few types of tumour – potentially systemic, i.e. can affect all parts of the body. Therefore we need information about the individual spread pattern of the disease for the entire body. The radiologist plays a key role here. The advances in imaging procedures, such as Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET) and hybrid systems (PET/CT) allow a quick overview of the tumour spread in a diseased body. This represents a great progress and a change of paradigm in medicine: we don’t work with a focus on organs but on the disease itself.
Molecular imaging
Onco-diagnostic research puts a lot of emphasis on the development of procedures for the simultaneous imaging of morphological, biological and functional tissue characteristics. The term ‘molecular imaging’ comprises all those imaging procedures that facilitate the imaging of molecular structures or biological processes with the help of suitable markers and also allow a quantitative evaluation. The objective is to gain information about a tumour, such as tumour biological functions like cell division or the formation of blood vessels which supply the tumour. The technical integration of PET and CET already proved clinically significant for oncology shortly after its introduction in 2001 as it enables us to assign tumour-specific functional changes (PET) to anatomical structures (CIT).
Progress MRI
The development of high resolution whole body MRI has resulted in a further, important progress for onco-diagnostic radiology. Comparative studies of whole body MRI and whole body CT and PET/CT have shown the advantages of MRI, particularly for the detection of distant metastases in the cerebral area, the liver and bones. Moreover, radiologists are currently following and shaping the development of the MR/PET with excitement.
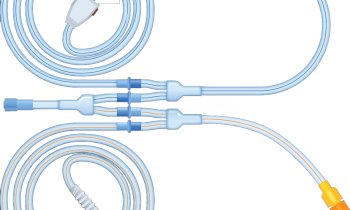
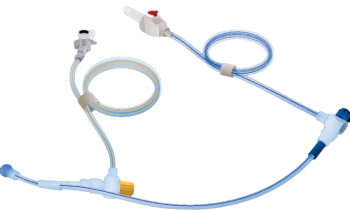
Interventional radiology
Radiologists can do more than ‘just’ diagnose. With interventional radiology, a fairly recent development within the field of imaging, they can actively take part in the therapeutic process. Image-guided minimally invasive interventions, such as tissue sampling, and localised therapy procedures, such as radiofrequency ablation or cutting off the blood supply of tumours (embolisation), are gentle and effective procedures of radiological cancer therapy.
Conclusion
Radiology now needs to combine methodical and clinical studies to examine the diagnostic efficiency and therapeutic relevance of modern imaging procedures. At the same time the challenges posed by the large volumes of image data, increasing time pressures and pressure to improve productivity, need to be mastered through more efficient examination procedures and increased competence. However, the most important factor is the specialist medical and personal exchange between radiologists and their clinical colleagues. The Radiology Congress offers an outstanding opportunity for this process. ”
01.05.2009