Article • Hygiene and microbiology meeting
No all clear for nosocomial infections
Experts at the 70th Annual Meeting of the German Society for Hygiene and Microbiology, held in Bochum, exchanged information on newly discovered resistances.

‘Specifically, resistance against a class of antibiotics that has, so far, always been viewed as a reserve appears to be developing more intensively than previously assumed,’ explained Professor Sören Gatermann, congress president and head of the Department for Microbiology at Ruhr University Bochum. The cause of resistance are different enzymes which make the antibiotic ineffective; its identification needs the most up-to-date molecular procedures, to determine which medication will be effective for a certain patient. There is another class of resistances causing concern among scientists. Mutations in the bacterium itself lead to certain antibiotics becoming ineffective. These resistance mechanisms, which were neither acquired nor depend on inactivating enzymes, are occurring increasingly. The European Committee on Antimicrobial Susceptibility Testing (EUCAST) determines the limits up to which a bacterium is still considered treatable with antibiotics. New resistances are often hard to detect, Gatermann explained, ‘so we must work on a genetic level to determine which treatments are likely to be effective for a patient.’
Cause of resistances and regional variations

Therapy with antibiotics is the only treatment to affect not only the patient treated but also all other patients. If an antibiotic is used in the intensive care unit (ICU) this not only affects the bacteria of the treated patient but also the entire hospital and its environment. This leads to different resistance profiles that can vary significantly from country to country. However, in-patient facilities account for a relatively low proportion (10-20%) of the overall daily doses of antibiotics administered. Antibiotics are far more commonly prescribed in out-patient care. There are also big regional differences: In the East of Germany the prescription rate is low, with the highest daily doses being prescribed in the Saarland, although this represents only half of the prescriptions in France.
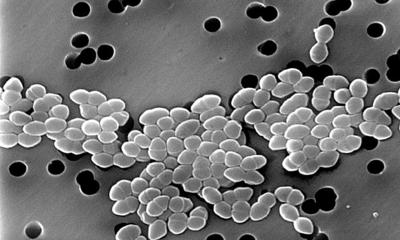
‘Each patient enters hospital with between two to three kg of bacteria. Up to 10% of the population already carry multi-resistant pathogens on admission,’ explained Professor Frauke Mattner, congress president and Head of the Institute for Hygiene at the Cologne Municipal Hospitals Group. The origin of the pathogens is still unclear. It is likely that they do not originate in drinking water but are spread through food, foreign travel or intensive animal farming. A certain proportion may also be spread from patient to patient in medical facilities. Which of these causes represents which proportion of the colonisation should be the subject of research to help tackle the problem in the future.
Comprehensive screening is not helpful
Wrong determination of resistance can also have severe consequences in the case of MRSA, as the patient is not given the correct antibiotic. The probability is 1:1. This means that every other patient may receive incorrect treatment
Sören Gatermann
The congress presidents agreed that comprehensive screening of patients for MRSA and multi-resistant gram-negative bacteria on admission is a waste of financial and staffing resources as well as counter-productive. Although patients in more frequent contact with hospitals and care facilities are at higher risk of colonisation with MRSA, pure MRSA screening would take no account of other pathogens. Each individual hospital should determine which risk groups typically prevail in their facility and should then decide which type of screening and procedures are likely to be effective. This approach corresponds with the evidence-based recommendations from the Robert-Koch Institute (KRINKO).
Gatermann explained that higher staff levels and adherence to hygiene regulations are more effective than screening all patients, particularly for multi-resistant gram-negative bacteria. Also, the diagnostic sensitivity for gram-negative pathogens is not particularly high, with patients sometimes having to be examined over and over again.
General screening could lead to say 400 patients declared as being colonised when, in reality, only one is, Gatermann explained. A screening requirement would therefore lead to inadequate care for 399 patients. It would be better to carry out specific screening based on the epidemiology and risk group for whom the most benefit can be expected. ‘Wrong determination of resistance can also have severe consequences in the case of MRSA, as the patient is not given the correct antibiotic. The probability is 1:1. This means that every other patient may receive incorrect treatment.’

More university education and academisation of care
Hospital hygiene has experienced staff shortages in Germany for years. Around 1,000 specialists for hospital hygiene are required. However, universities are not being encouraged, and Chair of Hygiene positions are only filled with delays or not at all. Only 7 out of 35 medical faculties have a department chair of hygiene and epidemiology. However, there has been considerable improvement over the last few years in the recruitment of hospital hygiene professionals. In North Rhine-Westphalia for instance the coverage is now at 90% of the KRINKO capacity recommendation. But Frauke Mattner sees a need for action by international comparison: ‘Germany brings up the rear in the ratio between nursing staff per patient, and we have the least academic staff. But it has been proven that an increase in the number of nursing staff with academic qualifications can reduce the number of nosocomial infections by 20 – 30%. This was evaluated across Europe in the 2014 RN4Cast Study. The newly designed nursing training programmes neglect academisation. They have increased quantity at the cost of quality, but both are required.’
Profiles:
After gaining her medical degree, Professor Frauke Mattner MD trained in Laboratory Medicine in Hamburg and then specialised in Hygiene and Environmental Medicine at Hanover Medical School (MHH), with habilitation completed in 2007. In that year she also became head of the Hygiene Department at the Institute for Medical Microbiology and Hygiene, Lübeck University Hospital. Since 2010, the professor has headed the Institute for Hygiene at the Cologne Municipal Hospitals Group, University Hospital Witten-Herdecke, Campus Cologne Merheim, and was appointed adjunct professor at the MHH in 2012.
After receiving his doctorate, Professor Sören Gatermann began his career as a research associate at the Institutes for Microbiology at universities of Hamburg and Lübeck. His habilitation in Medical Microbiology was completed in 1991 and he received the Venia Legendi and specialist accreditation in 1992. Two years later he was awarded a C3 professorship at Mainz University. The professor has been Chair of Medical Microbiology at the Ruhr University Bochum since October 1997. From 2009 he has also headed the National Reference Laboratory for Multidrug-resistant Gram-negative Bacteria, and became head of the National Antimicrobial Susceptibility Testing Committees (NAK), the German branch of EUCAST, in 2014
23.04.2018