News • Antiviral design
CAR-T gene therapy could provide long-term HIV protection
Findings
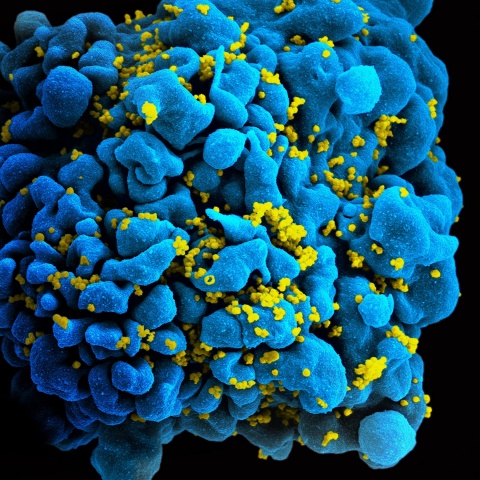
Through gene therapy, researchers engineered blood-forming stem cells (hematopoietic stem/progenitor cells, or HSPCs) to carry chimeric antigen receptor (CAR) genes to make cells that can detect and destroy HIV-infected cells. These engineered cells not only destroyed the infected cells, they persisted for more than two years, suggesting the potential to create long-term immunity from the virus that causes AIDS.
Background
Antiviral drugs can suppress the amount of HIV in the body to nearly undetectable levels, but only an effective immune response can eradicate the virus. Researchers have been seeking a way to improve the body’s ability to combat the virus by engineering blood-forming stem cells to specifically target and kill HIV-infected cells for the life of the individual. Although chimeric antigen receptor (CAR) T-cells have emerged as a powerful immunotherapy for various forms of cancer – and show promise in treating HIV-1 infection – the therapy may not impart long-lasting immunity. Researchers, physicians and patients need T cell-based products that can respond to malignant or infected cells that may reappear months or years after treatment.
Method
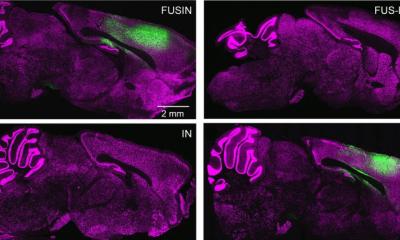
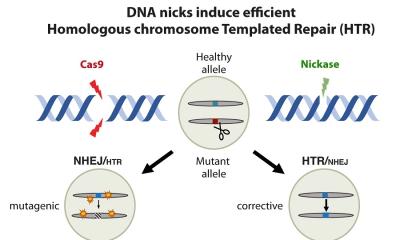
Because HIV uses CD4 to infect cells, the researchers used a CAR molecule that hijacks the essential interaction between HIV and the cell surface molecule CD4 to make stem cell-derived T-cells target infected cells. When the CD4 on the CAR molecule binds to HIV, other regions of the CAR molecule signal the cell to become activated and kill the HIV infected cell. The researchers found that, in test animals, modification of the blood-forming stem cells resulted in more than two years of stable production of CAR-expressing cells without any adverse effects. In addition, these cells were widely distributed throughout the lymphoid tissues and gastrointestinal tract, which are major anatomic sites for HIV replication and persistence in infected people. Most important, engineered CAR T-cells showed efficacy in attacking and killing HIV-infected cells.
Impact
These findings are the first to show that blood-forming stem cells can be modified with a CAR therapy that can safely engraft in the bone marrow, mature and become functional immune cells throughout the body. This could lead to the development of an approach allowing for safe, lifelong immunity to HIV. Such an approach is likely to work best when performed in combination with other treatment strategies, such as antiretroviral therapy. Researchers hope that this type of therapy could reduce infected individuals’ dependence on antiviral medications, lower the cost of therapy, and permit the possible eradication of HIV from its hiding places in the body. The approach also has potential against other infections or malignancies.
Authors
Study authors are Anjie Zhen, Mayra Carrillo, Cindy Youn, Brianna Lam, Nelson Chang, Heather Martin, Jonathan Rick, Jennifer Kim, Nick Neel, Valerie Rezek, Masakazu Kamata, Irvin Chen, Jerome Zack, and Scott Kitchen of UCLA; Christopher W. Peterson and Hans-Peter Kiem of the Fred Hutchinson Cancer Research Center and the University of Washington in Seattle; and Sowmya Somashekar Reddy of the Hutchinson Center.
Source: University of California, Los Angeles (UCLA), Health Sciences
31.12.2017