Article • Big Data
‘Dr Computer’ aids intelligent lung cancer diagnoses
In imaging diagnostics computers are taking over – well, not quite, but they might soon play an important role, according to Professor Hans-Ulrich Kauczor, Medical Director of the Clinic of Diagnostic and Interventional Radiology at University Hospital Heidelberg. Meeting with European Hospital, he discussed an EU-funded project to assess malignancy in pulmonary nodules and its implications for the radiologist’s profession.
Asked whether the computerised assessment of pulmonary nodules is on the way, Kaucsor confirmed: ‘Colleagues from Oxford and Groningen and our team are indeed working on using computer algorithms based on CT images to detect and characterise pulmonary nodules. We submitted the proposal for EU funding and received a favourable response.
‘Thus, we expect the project, to be known as ‘Lucinda’, to start next year. It aims to develop a method for intelligent lung cancer diagnosis.
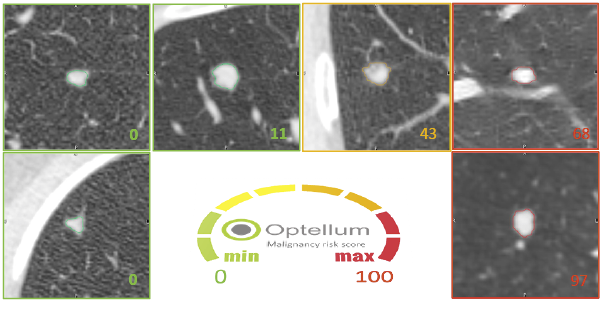
‘The task at hand is to validate the performance of an algorithm, which was initiated by a team at Oxford University Hospital headed by Fergus Gleeson and then further developed by Optellum, a spin-off company. Preliminary tests and publications are promising.
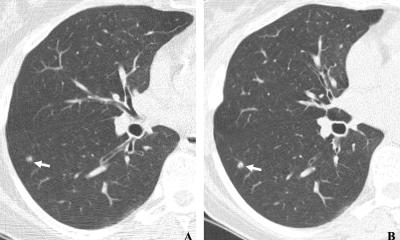
‘The idea is to use Big Data and machine learning. We’ll have to assess whether the programme also works with images from different sources, such as different scanners, and with different slice thicknesses and different reconstruction algorithms. We will contribute a set of CT images of the lung with a validated diagnosis of pulmonary nodules. The images were acquired in our Heidelberg lung cancer screening cohort LUSI and in clinical routine at the Thorax Clinic of Heidelberg University Hospital. The colleagues from Groningen will draw on the Nelson cohort, a Dutch-Belgian lung cancer screening cohort.
‘We aim to collect 2,000 data sets. We hope, when reading the 2001st data set, the algorithm will tell with 90 percent specificity whether the tumour is malignant or benign.’
Could a computer alone come p with a diagnosis?
Machine learning is a promising option for the radiologist to get help with the basics.
Prof. Hans-Ulrich Kauczor
‘The computer will facilitate our work – and that reflects the fact that there are fewer and fewer experts in this highly specialised area. As radiologists, we want the machine to do the groundwork but we’ll remain the ones to make the final decision.
‘If the radiologist turns into a mere report generator, the discipline will lose its charm and the profession will lose its attraction. Nobody wants to be in a profession where the mark of distinction is the ability to read 1,000 images or more a day. To diagnose more patients with more images in less time – that is not going to improve quality.
‘Machine learning is a promising option for the radiologist to get help with the basics. But in the end the machine cannot evaluate the results it generates. The role of the radiologist will move towards placing the results in a context, evaluating and communicating them.
‘For example, an algorithm that can reliably assess a pulmonary nodule can be used very well for screening purposes. The primary aim is to find out whether we are dealing with a malignant tumour or whether the lesion might become malignant. If a lesion is found to be malignant it is the task of the radiologist to refer the patient for further diagnostic work-up and therapy along the clinical path.
‘The clinical situation, however, is fraught with a number of challenges. Let’s say the patient is sick and presents with different comorbidities. Then we have to evaluate the images in their clinical context, help the referring physician to determine the right therapy and follow up on it. Machine learning systems cannot handle this type of complexity in the clinical environment.’
Will the profession now known as ‘radiologist” change?

‘We have to move from volume-based to value-based radiology. The American College of Radiology faces this challenge with its Imaging 3.0 strategy, which aims to integrate contact with the patient and his or her family much more tightly in the work of the radiologist. I consider this to be of utmost importance.
‘Our very dense and optimised workflows confuse the patient: he sees five physicians who give him four different explanations.
‘The radiologist’s clinical services should be performed reliably and the relevant information should be provided to all parties involved in a comprehensible and usable manner. Not every physician in the treatment context has to actually see the patient.
‘As far as I’m concerned, the challenge for the profession “radiologist” and the advanced training is not to consider computers a black box, but to master them. We have to know our systems. What input do we provide and what the output is going to be? How do we acquire images? Which protocol am I to use and why? What is the function of contrast media? To what extent can I rely on the results? This is the core of the discipline: interpretation and decision making. ‘We cannot ignore the trend towards Big Data – and we don’t want to. As radiologists we pioneered the integration of IT and PACS and have proven to be innovative.
‘Unfortunately, during the past five years we have lost ground. I think that is a big mistake. We are, and should remain, the experts when it comes to image data, networking, interpretation, decision-making and associations. This is where we have to look for a sustainable definition of our role.’
Profile:
Since 2008 Hans-Ulrich Kauczor has been full Professor and Chairman of Radiology at the University of Heidelberg and Medical Director of Diagnostic and Interventional Radiology at the Heidelberg University Hospital. He has also been Principal Investigator of the Translational Lung Research Centre in Heidelberg (TLRC) and, since 2012, the German Centre for Lung Research (DZL).
25.11.2016