Therapy
New way to predict COPD progression
New research has found that a process initiated in white blood cells known as neutrophils may lead to worse outcomes for some patients with chronic obstructive pulmonary disease (COPD). The discovery may help identify patients at higher risk for COPD progression, who might also show little benefit from standard treatments.
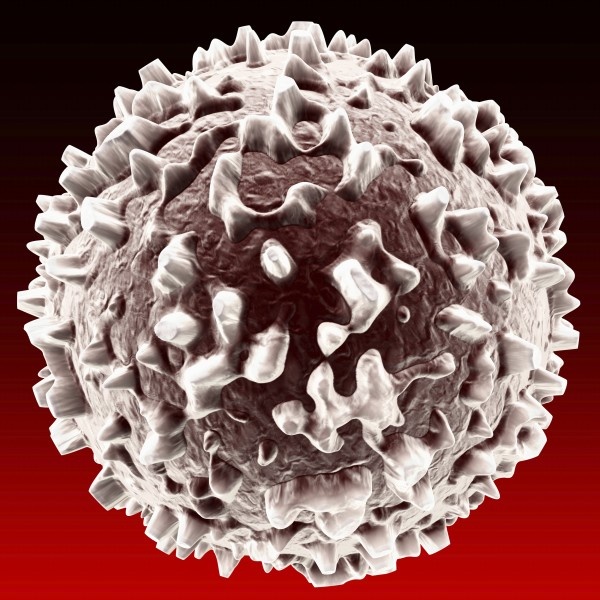
“We have known for many years that neutrophils should be able to fight infection, but we haven’t fully understood why they don’t work in COPD,” said lead author James D. Chalmers, MD, PhD, from the University of Dundee, Scotland. “Our study found that a recently identified form of neutrophil behavior called neutrophil extracellular trap (NET) formation is present in the lungs of COPD patients, and may weaken their ability to eat and kill bacteria.”
Dr. Chalmers noted his team found that when NET formation weakens neutrophils’ bacteria-fighting capability, patients experience more frequent chest infections and worse lung function and quality of life.
“This marker may help us identify patients at higher risk of disease progression,” he said. “And it identifies a subset of patients who may need treatments other than corticosteroids. Our data show that inhaled steroids may even exacerbate NETs, so we need to identify new COPD treatments and discover whether inhibiting NET formation will result in improved clinical outcomes for patients with COPD.”
Dr. Chalmers and colleagues recruited 141 patients with stable COPD for the study. Sputum and blood were collected at the beginning of the study, during acute COPD exacerbations, and at the end of exacerbations. NETs were measured using a validated enzyme-linked immunosorbent assay targeting specific DNA associated NET/protein complexes.
The amount of NET complexes in the lungs of patients in the study was directly related to the severity of their COPD and the risk of exacerbations. NETs increased significantly during exacerbations that did not respond to corticosteroid treatment.
Neutrophilic airway inflammation has been known for some time to be a characteristic feature of COPD. NETs were discovered as an essential part of innate immune response to infection approximately 10 years ago, and scientists are only beginning to understand how NETs impact disease outcomes.
“Some recent studies described the presence of NETs in the COPD lung, so we wanted to know whether there was any relationship between NETs and outcomes in COPD patients,” said Dr. Chalmers. “We are now keen to find out if we can identify why NET formation occurs in these patients and whether it can be prevented or treated. While our new research is at an early stage, we hope that detecting NETs may be a biomarker that can identify patients at risk of deterioration, and that we can work toward testing whether inhibiting NET formation would be a beneficial treatment in COPD.”
Source: American Thoracic Society (ATS)
18.05.2016











