Article • Cases rise
Should we screen for sickle cell disease?
Every year around a quarter of a million children worldwide die from sickle cell disease. In Germany around 3,000 people suffer from this rare inherited blood disorder.
Report: Sylvia Schulz
However, the trend is rising: the influx of refugees is most probably linked to this increase, since the disease exclusively affects those from a migrant background.
Patients who do not have sickle cell disease diagnosed in time often die in childhood or adolescence. In countries such as the USA, The Netherlands and France tests for this disease are already part of standard newborn screening.
The families of those affected originate from areas where Malaria has been, or still is, endemic. The prevalence is highest in West Africa. In this region, every fifth death amongst children under the age of five is caused by sickle cell disease.
Testing for sickle cell may become routine for babies

In countries such as Germany early detection is currently not assured. However, three model projects in Berlin, Hamburg and Heidelberg have now been set up to find out whether testing for sickle cell disease can and should become part of regular newborn screening.
Only once the disease has been diagnosed can the appropriate treatment commence. ‘Even very simple measures can reduce the impact of the disease and the high early mortality rates drastically,’ point out Dr Stephan Lobitz of the Clinic for Paediatrics, Division of Oncology and Haematology at the Charité Hospital in Berlin, one of the three centres participating in the study. ‘Educating parents to recognise acute anaemia and to seek medical help quickly if a child develops a fever, along with prophylactic treatment with penicillin and vaccinations, can prevent almost all related deaths in childhood and adolescence.’ However, a prerequisite for this is that the blood disorder has been diagnosed and that the parents have been informed about it. Therefore, Lobitz believes, standard newborn screening is essential.
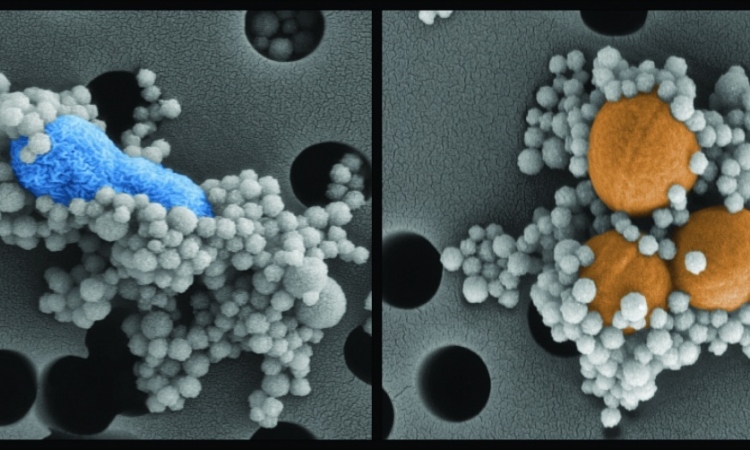
Sickle cell anaemia results from inherited changes to the haemoglobin in red blood cells (erythrocytes). The most important function of haemoglobin is to carry oxygen from the lungs to organs and tissues. Erythrocytes are filled with fluid and haemoglobin usually remains dissolved in this fluid.
Erythrocytes can be deformed
However, the haemoglobin of patients with sickle cell anaemia clumps together into solid structures inside the erythrocytes once it has released the oxygen and loses its functionality. These solid structures impact on the usually very high flexibility of the erythrocytes and damage the cells, shortening their lifespan. As a result, the erythrocytes become deformed, remain in small blood vessels and block them. This leads to small infarctions and very small damage to the organs, which, over time, can add up and in turn lead to a significant impairment to the function of certain organs, and even their total destruction. Simultaneously, the premature death of blood cells causes an increased accumulation of metabolic products, which in turn can damage larger blood vessels.
Along with these slow, but steadily progressive changes there are also acute problems caused by the sudden accumulation of large numbers of sickle cells.
Screening with tandem mass spectrometry
German laboratories are usually not equipped with the devices that are used internationally
Stephan Lobitz
These so-called crises, the triggers of which are not yet entirely clearly defined, often go hand in hand with severe pain, frequently can only be treated in hospital and should be treated with the strongest painkillers, severely impacting on quality of life. There are other acute and serious complications, such as splenic sequestration, where blood only flows into the spleen but not out again. Every ninth patient is destined to suffer a stroke before his or her 18th birthday. Viral infections can lead to acute, life-threatening anaemia.
The project is now examining whether testing for sickle cell disease in Germany is possible with standard laboratory procedures. ‘German laboratories are usually not equipped with the devices that are used internationally,’ Lobitz reports. However, he believes that tandem mass spectrometry, which is usually part of standard screening in this country, could also be used to diagnose sickle cell disease. ‘We would have to ensure that reliable results are available fast and that the affected newborns can be transferred quickly to wards that specialise in the treatment of blood disorders,’ he emphasised.
So far, 90,000 children have been examined in the context of screening at the three locations (Hamburg, Heidelberg, Berlin); 24 were confirmed with sickle cell disease. It is not yet clear how the findings will be translated into actions. The relevant political negotiations are currently taking place, Lobitz reports. Researchers are also receiving support from the German Society of Internal Medicine (DGIM). ‘The most important concern for DGIM members is also to find solutions for the best possible diagnosis and treatment for diseases that only affect a relatively small number of people,’ says Professor Ulrich Fölsch, General Secretary of the DGIM from Kiel. Therefore the DGIM welcomes advances made by this research group.
Profile:
Dr Stephan Lobitz works in the Clinic for Paediatrics, Division of Oncology/Haematology at the Charité Hospital Berlin. After completing his medical degree at the Heinrich-Heine University in Dusseldorf he worked as a research associate at the Charité Paediatrics Clinic. He has specialised in Paediatric Medicine since 2012 and is also a Speaker for the management of the GPOH (Society for Paediatric Oncology and Haematology) Sickle Cell Disease Registry Study.
22.03.2016