Risks from cold and dry gas insufflation become history
Modern laparoscopy, the technique of looking inside the abdominal cavity, is a major medical innovation driven initially by physicians from Germany as well as by Swedes and Americans.

Following its inception, around 1900, the technique found its way into routine clinical practice. Use of a video camera mounted on the laparoscope greatly facilitated minimally invasive methods in the 1980s: manipulating the scope was managed by a second person and images displayed on a monitor freed the surgeon’s hands.
Pumping gas (‘insufflation’) creates space to provide visibility and room to move. However, serious issues remained unsolved, as Dr Jonathan Sackier from the University of Virginia explained at a recent event in Berlin, Germany addressing top surgeons from renowned hospitals. The gas used for these procedures, he pointed out, is conventionally delivered cold and dry, potentially harming the patient, and one of the numerous medical technology innovations in emanating from New Zealand now helps avoid the problems caused by ‘cold and dry’ insufflation.
‘Physicians should never forget the lessons they have learned in surgery or indeed in any other discipline,’ Dr Sackier stressed. ‘However, there are new lessons to be understood, and we should all use our best judgment for the benefit of all our patients’. Laparoscopy, over the years, has turned out to be a brilliant approach; it allows patients to leave hospital sooner, and significantly reduces postoperative pain. However, several issues remain: ‘The established standard has been to fill the abdominal cavity with carbon dioxide creating a pneumoperitoneum or gas-filled space. In our laboratory, we studied the effects on the peritoneum and general physiology of inflating with cold and dry gas.’
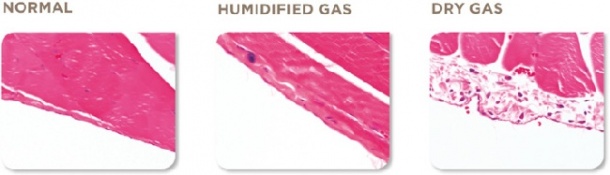
Cold and dry gas kills cells
In various countries, regulations rule out intra-operative cooling, he explained. In open surgery, warm and moist pads are used to pack away organs; this is done to avoid exactly the effects that, in laparoscopy, cold and dry gas produces: fat dries out and darkens, organ surfaces blanch and swell, cells desiccate and die. ‘Look at the peritoneum’, Dr Sackier pointed out. ‘It’s a very delicate monolayer, which covers a surface area larger than the skin. Damage to the peritoneum causes pain and inflammation and can lead to adhesions.’
So, while laparoscopy was inspired by reducing the harm physicians do, insufflation of gas at an average temperature of 15°C and zero humidity causes morbidity, the possibility of impaired fertility and even increased mortality in the medium and long term.
Warm and wet should become the gold standard
‘Warming and humidifying insufflated gas, serves to significantly limit the negative effects which I have described,’ he continued. ‘The technology now in use delivers water molecules mixed in with the gas – very clever!
‘Fisher and Paykel Healthcare have developed a device that suits these requirements; it helps to improve core body temperature, reduces pain and adhesions, speeds recovery and return to normal activities.’
Good surgical practices, Dr Sackier believes, clearly favour deploying this easy-to-use device.
Professor Jürgen Kleinstein, Director, Magdeburg University Hospital for Reproductive Medicine and Gynaecological Endocrinology, agrees: ‘We’ve been using the system from Fisher & Paykel and have seen very good results, for example a reduced number of adhesions. During the procedure, benefits include a smaller amount of narcotics is needed, because the stimulus targeting the peritoneum is reduced… We will not do laparoscopic procedures without this system from Fisher & Paykel Healthcare; I strongly recommend colleagues should embrace it.’
Profile:
Surgeon Jonathan Sackier MD has helped to introduce laparoscopic techniques and his studies have been widely published. He left the UK to work at the George Washington University, Washington, D.C. where he co-founded the Washington Institute of Surgical Endoscopy. There, in addition to research activities, students and residents, as well as physicians from all over the world, are taught laparoscopy techniques. Today, he is Professor of Surgery and Medicine, teaching at the Department of Surgery at the University of Virginia in Charlottesville.
26.08.2013











