Routine clinical use will take another decade
A tissue plaster for the infarction scar
Numerous cardiac muscle cells die following myocardial infarction, due to reduced blood flow in the affected muscle areas. What remains is a scar, which also mechanically affects cardiac pumping. The muscle itself has no, or hardly any, capacity to regenerate itself.

Speaking at the Annual Meeting of the German Cardiac Society in Mannheim this April, Professor Gerd Hasenfuss, head of the Göttingen Heart Research Centre, explained, ‘At best, the heart has a capacity of around 1% to regenerate itself.’ Although this means that the heart completely renews itself once throughout a person’s entire lifetime, this capacity is not nearly strong enough to counteract any damage occurred during acute events.
There have therefore been – and still are – high hopes placed on potential stem cell therapy. Pluripotent cells are to replace damaged tissue. The initial phase, when expectations of this therapy were rather exuberant, appears to have passed for now, although the first case studies of catheter-supported application of stem cells from the bone marrow for patients who have just suffered heart attacks were still being hailed as recently as 2000. Meta-analysis, Prof. Hasenfuss pointed out, has shown that, although the application of bone marrow stem cells after a myocardial infarction results in a slight improvement of cardiac function, the effect could later no longer be verified. ‘The stem cells cannot differentiate. So it’s assumed that what can initially be seen is in fact a slight “pharmacological” effect of the bone marrow stem cells - they may be secreting messenger substances with a supportive impact on tissue regeneration.’ New opportunities for stem cell therapy are therefore the object of much research. One option being more extensively examined is the use of cardiac progenitor cells. ‘Small amounts of these cells can be found in the heart,’ explained the Göttingen cardiologist. These stem cells are harvested via biopsy. Because only few cells are naturally available, the cells have to be grown in vitro, making this approach unsuitable to treat acute infarctions. Moreover, clinical studies confirming the effectiveness of the procedure are lacking. Based on today’s level of knowledge, Prof. Hasenfuss sees the best chances for stem cell therapy in the use of induced pluripotent stem cells. In 2012, Japanese doctor and scientist Shin’ya Yamanaka and British researcher Sir John B Gurdon received the Nobel Prize for their discovery that mature cells can be changed into stem cells. Prof. Hasenfuss: ‘Practically every cell in the body is interconvertible.’
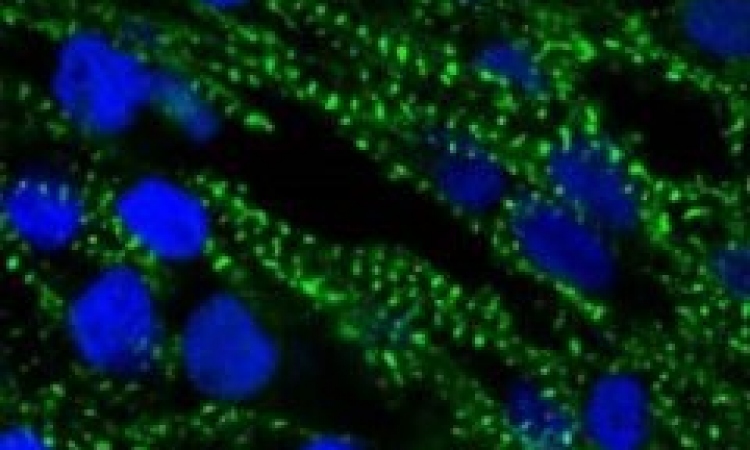
This means, for example, heart or liver cells can be grown from skin or blood cells. The mature cells are basically reprogrammed back to the stage of stem cells and are then differentiated into heart muscle cells, for instance. The objective is to grow heart tissue using induced pluripotent stem cells, which can then be transplanted to areas affected by post-myocardial infarction scarring. This tissue plaster, so goes the idea, can then stabilise the infarction scar as well as improve the contractility of the myocardium. ‘This tissue engineering approach also facilitates better control of tumour growth,’ Prof Hasenfuss explains, highlighting another advantage compared to previous approaches in stem cell therapy. In addition, the new heart tissue would be grown in the laboratory under controlled conditions. However, it will be a while before this procedure will become part of clinical routine. It is now possible to create cell layers. Whether or not these will have the desired characteristics is currently being trialled in animal experiments. The first human studies could, he estimates, take place in five years’ time. Based on a positive progression of studies and trials it will take at least another decade for the procedure to be ready for clinical use.
Based solely on his looks, Professor Gerd Hasenfuss could be classed as an eternal youth among cardiologists. However, he can in fact look back on an impressive career, having taken on outstanding leadership roles early in his medical career. The professor studied medicine and specialised in cardiology in Freiburg, Germany. Following research in the USA he wrote his habilitation in 1989. In 1993 he became a consultant and in 1996 was awarded an extraordinary professorship. He was awarded a C-4 professorship at Göttingen University and then appointed Director of the Cardiology and Pulmonology Departments at the Centre for Internal Medicine. Since 2001 he has also chaired the Göttingen Heart Research Centre and, since 2005, been head of Internal Medicine at the Lippoldsberg Rehabilitation Centre.
07.05.2013