Image source: Nephron, Diffuse large B cell lymphoma - cytology low mag, (CC BY-SA 3.0)
News • Diffuse Large B-Cell Lymphoma (DLBCL)
Personalised simulations predict outcomes for blood cancer treatment
A new study led by researchers at Brighton and Sussex Medical School (BSMS) has unveiled a groundbreaking approach to predicting the effectiveness of treatments for patients with Diffuse Large B-Cell Lymphoma (DLBCL), a common form of blood cancer.
The researchers utilised genomic sequencing data to create personalised simulations of individual patients that can quantify the impact of genetic mutations on cancer cell behaviour. This method promises to pave the way for personalised medicine, which will revolutionise clinical decision-making and advance care for heterogeneous blood cancers.
The study has been published in Nature’s Blood Cancer Journal.
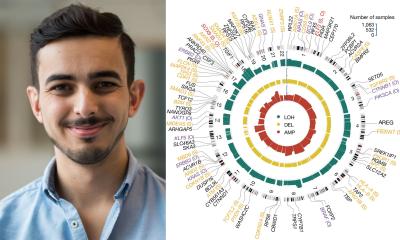
The research team, led by Dr Simon Mitchell, Reader in Cancer Systems Biology at BSMS and funded by Leukaemia UK and UKRI, focused on leveraging genomic data from DLBCL patients to simulate how specific mutations affect anti-apoptotic and pro-proliferative signalling within cancer cells. Unlike traditional approaches that rely on mutational clustering, the simulations provided a more comprehensive understanding of the interplay between multiple mutations. Rather than grouping patients sharing common mutations, their approach groups patients based on the impact of mutations within complex signalling networks.
As [genomic] sequencing costs decrease, we hope that this approach will become a standard diagnostic practice, enabling precise identification of patients who might benefit from alternative treatments
Simon Mitchell
The study found that personalised simulations successfully identified patients with varying prognoses (dismal, intermediate and good) across multiple datasets. This was achieved using data from whole-exome sequencing (WES) or targeted sequencing panels, providing robust predictions despite the mutational heterogeneity. Unlike many statistical approaches, the predictive accuracy of the simulations improved with larger validation datasets, emphasising the importance of integrating molecular network knowledge into the analysis. The models were particularly effective at pinpointing patients with co-occurring mutations that promote both cancer cell proliferation and resistance to apoptosis – and found patients that would be missed by traditional clustering methods.
Commenting on the study, Dr Mitchell said: “This study supports the integration of genetic sequencing at the diagnosis stage of DLBCL to better determine patient prognosis. As sequencing costs decrease, we hope that this approach will become a standard diagnostic practice, enabling precise identification of patients who might benefit from alternative treatments. This study marks a significant step forward in the quest for personalised cancer treatment. By harnessing the power of computational modelling to place genomic data into the context we hope to pave the way for more accurate prognostic predictions and tailored therapeutic strategies. We believe such approaches promise a new era of precision medicine for blood cancer patients and potentially many others.”
Dr Simon Ridley, Director of Research & Advocacy at Leukaemia UK, added: “We are thrilled to have supported Dr Mitchell and his team’s new work. This study represents significant progress toward stratified medicine, enabling more targeted treatments that could lead to substantial improvements in the treatment of patients diagnosed with blood cancer. By using computational tools to model different patients' blood cancers, clinicians could eventually predict which patients will respond best to various treatment types. This work is a great example of what can be achieved through Leukaemia UK’s John Goldman Fellowships, where we strive to fund the most innovative early-career researchers with the potential to accelerate progress in blood cancer research.”
Beyond DLBCL, the computational modelling techniques demonstrated in this study have the potential to be applied to other types of cancer, particularly those characterised by high genetic heterogeneity. As genomic data becomes more widely available and computational methods continue to evolve, these personalised simulations could play a critical role in the era of precision medicine, tailoring treatments to individual genetic profiles for better patient outcomes.
Source: Brighton and Sussex Medical School
17.07.2024